Why I don't do vaginal exams ~ Wisdom from a Traditional Birth Companion
I let my new client know what would happen when I arrived at her home when she was in labour. We talked about sanitation measures, spending time in the kitchen, setting up the pool, and where I could take a nap if she needed some privacy. I said I would not be doing any vaginal exams as I think they’re rude, and she wept with relief.
I specialise in trauma and the majority of my clients are refugees from the medical system, running from ritual abuse and routines that protect the industry. They want someone to mentor them through to a healthy birth without the traps and trappings of the industry that removed their choice, and violated their autonomy and their dignity.
As a traditional birth attendant, I don’t do vaginal exams.
I was talking with my new client about what would likely happen when I arrived at her home when she was in labour. We talked about sanitation measures, spending time in the kitchen, setting up the pool, and where I could take a nap if she needed some privacy. I said I would not be doing any vaginal exams as I think they’re rude, and she wept with relief.
I specialise in trauma and the majority of my clients are refugees from the medical system, running from ritual abuse and routines that protect the industry. They want someone to mentor them through to a healthy birth without the traps and trappings of the industry that removed their choice, and violated their autonomy and their dignity.
We won’t go into the history of obstetrics that began with the burning of witches (midwives and healers), the rise of the man-midwife, the development of lying-in hospitals, and eventually the wholesale co-opting and medicalisation of birth. Suffice it to say that obstetrics and hospitalisation didn’t “save” women and babies (1). It created untold harm and mortality until they learned better infection control and saner behaviours. Today, it’s still leaving a trail of destruction as about 1/3 of their clients are traumatised (2,3,4) and about 1 in 8 enter parenthood with postpartum post-traumatic stress disorder (5,6,7). Suicide is a leading cause of maternal death in the first year and is highly correlated to trauma (8,9,10,11,12,13,14,15,16). It’s an industry out of control with unjustifiable caesarean rates, dangerous inductions for spurious reasons, and wholesale overuse of medications and interventions.
What women didn’t notice in this process of medicalisation and co-opting of their physiology for profit is that the medical industry took ownership of their vaginas once they became pregnant. Pregnancy transfers ownership of the vagina from the woman to the industry. Midwifery and obstetrical regulations stipulate that inserting an instrument, hand, or finger beyond the labia majora is a restricted practice sanctioned by legislation (17). To test this, see how long it takes for someone in the industry to file a Cease and Desist or start a campaign of persecution for the purpose of prosecution if they catch wind of anyone but one of their own sticking their fingers up there. No one but an insider sticks their fingers into their territory. It doesn’t matter who the mother gives her permission and consent to - it must be a member of the priesthood of modern medicine.
Of course, in their benevolence, they’re generally quite accommodating where partners are concerned, because most partners are male and obstetrics is exceedingly misogynistic. They value the needs and the pleasures of the D.
As a traditional birth attendant, I don’t do vaginal exams. For one thing, it’s considered a restricted practice for just the medical pundits and not doing them with my clients keeps the industry players somewhat placated knowing I’m not intruding into their turf. But the real reason is because I think they’re completely unnecessary and wouldn’t do them even if the medical folks begged me to under the guise that it would make birth safer.
To better understand the offence of the routine vaginal exam, we have to go back in time to when the male-midwife moved into the sanctity of women-centred birth and the domain of the midwife. It was profitable. And they convinced the public that they would provide a superior service based on the cultural belief of the time that women were disadvantaged by an inferior intellect and a predilection for sorcery (18,19). They also brought with them the medical perspective that women were an error of nature and that the world, and thus its inhabitants, were but a machine that could be best understood by coming to know its parts in isolation of the whole.
And so began dissection, mechanisation, and reducing birthing women to their parts. She became a womb expelling a foetus through a vagina. Think of today’s obstetrical “power, passenger, passage” perspective on how birth unfolds. Not much has changed in 400 years.
By sticking their fingers up there, they discovered that the cervix opens to expel the foetus. Oh, happy day! From the morgue to the birth suite, physician fingers were poking everything. Throughout the early and mid 1800’s, the infection rate in some hospitals soared as high as 60% from the mysterious childbed fever, with death rates as high as 1 in 4 (20). Nothing the doctors did was contributing to this mystery as physicians were gentlemen and gentlemen didn’t carry germs (21). And once they did accept that their filthy practices were killing women, rather than abandon the idiocy of penetrating their patients in labour, they eventually figured out how to make it less dangerous.
The practice of obstetrics has always been highly resistant to change and common sense. After all, they’ve had 400 years to figure things out and women are still birthing on their backs!
Once it was discovered that the cervix dilates as part of the labouring process, the medical industry has been fixated on that bit of tissue and made it the focus of their entire assembly line drive-through everyone-gets-what’s-on-the-menu service. That bit of tissue determines how the ward allocates services, whether the client will be permitted to stay, and how long she’ll be allowed to use their services before the next client needs the bed.
Thanks to Dr. Emanuel Friedman, who examined the cervices of 500 sedated first-time mothers in the 1950’s and plotted their dilation on a graph and matched it to the time of their birth – we now have the infamous Friedman’s Curve and the partogram.
© Evidence Based Birth
The partogram is a graph that plots cervical dilation and descent of the foetal head against a time-line. When the graph indicates that progress is slower than is allowable according to the particular chart chosen by their institution, then the practitioner is called upon to administer various interventions to speed things up to keep the labour progressing well, aka, profitably. Should these acceleration measures fail to produce a baby in a timely manner or cause foetal distress, then a caesarean section is the solution. “Failure to progress”, and the accompanying foetal distress that is often a consequence of those acceleration measures, are the leading causes of a primary caesarean (22).
Obstetrical partogram
In addition to clearing the bed for the next client, obstetrics has another reason for expediting labour. The more vaginal exams a woman receives, the greater the likelihood she’ll develop a uterine infection (23). So, once they start the poking, they need to get the baby out before their prodding adds another problem for them to solve.
In the absence of a medical situation, routine vaginal exams in labour are for the purpose of charting in order to maintain a medicalised standard of modern technocratic birth.
A labouring client will not be admitted to a hospital without a vaginal exam to determine if her dilation is far enough along for their services (unless she’s clearly pushing). And this isn’t necessarily a bad thing. Early admission to the hospital results in more interventions and more caesareans than later admission (24). This is a business and time is money.
A regulated midwife attending a homebirth will likewise perform a vaginal exam upon arrival at the client’s home to determine if the client is far enough along to warrant their limited resources and time by staying and beginning the partogram or leaving and waiting to be called back later. They must also follow the rules of the hospital at which they have privileges or their regulatory agency and transport for augmentation/acceleration if the partogram shows a significant variation.
All of this is predicated on the outdated and obsolete notion that women are machines and birth is a linear process. The only thing a vaginal exam reveals is where the cervix is sitting at that particular moment and how it’s interpreted by that particular practitioner. Women are not machines and birth is not linear. Just like any mammal, birth can be slowed, stopped, or sabotaged by an unfavourable environment or reckless attendants. I’ve said for years that it’s so easy to sabotage a good birth, it’s embarrassing.
“Years ago, I was with a first-time mother planning a family-centred homebirth. She was on the clock and had a deadline. At 42 weeks gestation, she had until midnight that night to produce a baby in order to have a midwife-attended homebirth. After that, she was expected to report to the hospital for a chemical induction. As her contractions built throughout the day, her preferred midwife arrived and labour was progressing well. She was enjoying the process and the camaraderie of her sisters-in-birth. Eventually, one of the vaginal exams revealed a cervical dilation of 8 cm, indicating it was time to call in the 2nd midwife. Only, it was a midwife that had routinely upset the mother throughout pregnancy with requests for various tests and talk of all the dangers of declining routine testing. Upon learning this midwife was coming to the birth, labour slowed.
Soon enough, the 2nd midwife arrived and assumed authority over the birth process and insisted on repeated vaginal exams for the purpose of staying within the parameters of the partogram. Her vaginal exams were excruciating, no doubt because she was trying to administer a non-consenting membrane stripping as an intervention to address the slowed and almost non-existent contractions. Eventually, an exam revealed a dilation of only 6 cm. After several more hours of “torture” (according to this mother’s recount) to keep labour going rather than just leaving the mother to rest and accepting that this labour had been hijacked and needed time to regroup and restart, dilation regressed to 4 cm and the mother eventually ended up acquiescing to a hospital transfer, and experienced an all-the-bells-and-whistles birth, trauma, and postpartum PTSD.
This mother’s subsequent birth a couple of years later didn’t include inviting midwives and unfolded as it was meant to. After a day of productive and progressing labour that was clearly evident without sticking fingers up her vagina, she eventually got tired and labour slowed and stopped. She went to bed and I went home. When she woke up, labour resumed and a baby emerged swiftly and joyously. As it turns out, for her, she has a baby after a good sleep with people she trusts.”
What about the routine vaginal exams in late pregnancy? Glad you asked!
Since they don’t have good predictive value, meaning they won’t diagnose when labour will begin, how long it will take, or whether the woman’s pelvis will accommodate that particular baby prior to labour, they have 2 functions.
The first is to plan and initiate your induction.
A cervical exam provides information that is measured against a Bishop Score. A Bishop Score provides a predictive assessment on whether an induction is likely to result in a vaginal birth or is more likely to result in a caesarean for “failure to progress”. A cervix that scores higher is more likely to respond to an induction whereas a lower score indicates a less favourable outcome (25). Further, a vaginal exam allows the practitioner to begin the induction process with a membrane stripping/stretch-and-sweep.
The second purpose for routine vaginal exams in pregnancy is to build in sexual submission. It reaffirms the power dynamic where someone who is not the woman’s intimate sexual partner is allowed to penetrate her genitals at will. It makes their job much simpler once she’s is in labour. She has been trained to accept this violation.
A vaginal exam during labour might rarely be indicated when there is a problem that requires more information. A vaginal exam can help determine if there’s a possible cord prolapse requiring immediate medical attention, or can asses the position and descent of the baby to help suggest strategies to encourage the baby to move into a better position. However, when a labour is spontaneous, meaning it hasn’t been induced by any mechanical, chemical, or “natural” means, the labour isn’t augmented with artificial rupture of membranes or synthetic oxytocin, and the labouring woman is untethered and free to move as her body indicates, complications are far less likely.
Throughout my 35 years in supporting birthing families, I can say that babies do indeed come safely and spontaneously out of vaginas when there’s no one sticking their fingers up there. And they tend to come more quickly. Routine vaginal exams don’t contribute to the safety of the mother/baby. However, they do add to the safety of the practitioner who is tasked with placating the technocratic gods who demand they follow protocols and keep the wheels of the business running on track.
My reasons for not doing vaginal exams, even if the the technocratic gods gave their blessing, include:
They’re rude
They’re unnecessary
They shift the locus of power from the birthing woman to the person with the gloves
They introduce the potential for infection
They interrupt labour and can sabotage a good birth
They often hurt
They can traumatise the cervix
They can traumatise the mother
They can impact the experience of the baby
There are so many simpler ways to determine how labour is progressing
I don’t practice medicine or midwifery or engage in its absurdities
I really am not that interested in other people’s vaginas
Let’s talk about when labour does veer from a normal physiological process.
When the power dynamic places the labouring and birthing mother in charge of the experience, it actually becomes a safer and simpler process. She is the one who is experiencing the labour and birth and is the one relaying information. Only she is in direct communication with her baby. She is the one who knows when labour has exceeded her resources and she needs medical help, pharmacologic pain relief, or the reassurance of the technocratic model.
Of course, not all births unfold simply. However, my experience over these many years is that when women are not expected to submit to exams for the purpose of charting and the subsequent limitations imposed by those charts, birth unfolds a lot more simply far more often.
Much love,
Mother Billie ❤️
Endnotes
Tew, Marjorie. Safer childbirth?: a critical history of maternity care. (2013). Springer.
Garthus-Niegel, S., von Soest, T., Vollrath, M. E., & Eberhard-Gran, M. (2013). The impact of subjective birth experiences on post-traumatic stress symptoms: a longitudinal study. Archives of women's mental health, 16(1), 1-10.
Creedy, D. K., Shochet, I. M., & Horsfall, J. (2000). Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth, 27(2), 104-111.
Schwab, W., Marth, C., & Bergant, A. M. (2012). Post-traumatic stress disorder post partum. Geburtshilfe und Frauenheilkunde, 72(01), 56-63.
Montmasson, H., Bertrand, P., Perrotin, F., & El-Hage, W. (2012). Predictors of postpartum post-traumatic stress disorder in primiparous mothers. Journal de gynecologie, obstetrique et biologie de la reproduction, 41(6), 553-560.
Beck, C. T., Gable, R. K., Sakala, C., & Declercq, E. R. (2011). Posttraumatic stress disorder in new mothers: Results from a two‐stage US National Survey. Birth, 38(3), 216-227.
Shaban, Z., Dolatian, M., Shams, J., Alavi-Majd, H., Mahmoodi, Z., & Sajjadi, H. (2013). Post-traumatic stress disorder (PTSD) following childbirth: prevalence and contributing factors. Iranian Red Crescent Medical Journal, 15(3), 177-182.
Oates, M. (2003). Perinatal psychiatric disorders: a leading cause of maternal morbidity and mortality. British medical bulletin, 67(1), 219-229.
Oates, M. (2003). Suicide: the leading cause of maternal death. The British Journal of Psychiatry, 183(4), 279-281.
Cantwell, R., Clutton-Brock, T., Cooper, G., Dawson, A., Drife, J., Garrod, D., Harper, A., Hulbert, D., Lucas, S., McClure, J. and Millward-Sadler, H. (2011). Saving Mothers' Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG: an international journal of obstetrics and gynaecology, 118, 1-203.
Austin, M. P., Kildea, S., & Sullivan, E. (2007). Maternal mortality and psychiatric morbidity in the perinatal period: challenges and opportunities for prevention in the Australian setting. Medical Journal of Australia, 186(7), 364-367
Palladino, C. L., Singh, V., Campbell, J., Flynn, H., & Gold, K. (2011). Homicide and suicide during the perinatal period: findings from the National Violent Death Reporting System. Obstetrics and gynecology, 118(5), 1056.
Grigoriadis, S., Wilton, A.S., Kurdyak, P.A., Rhodes, A.E., VonderPorten, E.H., Levitt, A., Cheung, A. and Vigod, S.N. (2017). Perinatal suicide in Ontario, Canada: a 15-year population-based study. Cmaj, 189(34), E1085-E1092.
CEMD (Confidential Enquiries into Maternal Deaths) (2001) Why Mothers Die 1997–1999. London: Royal College of Obstetricians and Gynaecologists.
Sareen, J., Cox, B. J., Stein, M. B., Afifi, T. O., Fleet, C., & Asmundson, G. J. (2007). Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic medicine, 69(3), 242-248.
Hudenko, William, Homaifar, Beeta, and Wortzel, Hal. (July 2016). The Relationship Between PTSD and Suicide. PTSD: National Center for PTSD, U.S. Department of Veterans Affair.
Act, Ontario Midwifery. "SO 1991, c. 31." (1991).
Smith Adams, K. L. (1988). From 'the help of grave and modest women' to 'the care of men of sense': the transition from female midwifery to male obstetrics in early modern England. (Master’s thesis, Portland State University.
Burrows, E. G., & Wallace, M. (1998). Gotham: a history of New York City to 1898. Oxford University Press.
Semmelweis, I. (1983). Etiology, concept, and prophylaxis of childbed fever. Carter KC, ed. Madison, WI.
Halberg, F., Smith, H. N., Cornélissen, G., Delmore, P., Schwartzkopff, O., & International BIOCOS Group. (2000). Hurdles to asepsis, universal literacy and chronobiology-all to be overcome. Neuroendocrinology Letters, 21(2), 145-160.
Caughey, A. B., Cahill, A. G., Guise, J. M., Rouse, D. J., & American College of Obstetricians and Gynecologists. (2014). Safe prevention of the primary cesarean delivery. American journal of obstetrics and gynecology, 210(3), 179-193.
Curtin, W. M., Katzman, P. J., Florescue, H., Metlay, L. A., & Ural, S. H. (2015). Intrapartum fever, epidural analgesia and histologic chorioamnionitis. Journal of Perinatology, 35(6), 396-400.
Kauffman, E., Souter, V. L., Katon, J. G., & Sitcov, K. (2016). Cervical dilation on admission in term spontaneous labor and maternal and newborn outcomes. Obstetrics & Gynecology, 127(3), 481-488.
Vrouenraets, F. P., Roumen, F. J., Dehing, C. J., Van den Akker, E. S., Aarts, M. J., & Scheve, E. J. (2005). Bishop score and risk of cesarean delivery after induction of labor in nulliparous women. Obstetrics & Gynecology, 105(4), 690-697.
Birth Hijacked – The Ritual Membrane Sweep
I’ve written about many topics over the years but nothing has ever generated as much discussion, opposition, and vitriol as challenging the cherished routine membrane sweep/stripping, aka stretch-and-sweep. A few years ago, I wrote a post about how I’d like to see the routine, prior-to-40-weeks, without-medical-indication membrane sweep banned from obstetrical and midwifery practice. I talked about its risks and the fact that the clients I worked with called it a sexual assault when done without consent
The post went viral and I received hate messages and emails from around the world defending this procedure. In general, the sentiment was that I should most definitely be having sexual relations with myself, after which, I should be locked up and forever silenced. I also heard from hundreds of women whose births were ruined by days of painful, non-progressing contractions triggered by a membrane sweep that ended up in a fully medicalised all-the-interventions arrival for their baby that they didn’t want. And horrifically, even more hundreds wrote to share their stories of non-consenting, painful, and violating membrane sweeping when there was no reason for it, aside from the care provider’s decision that they had agency over their patient’s vagina and could do what they wanted when they wanted.
So what is it about membrane sweeping that is so cherished that challenging it generates death threats?
Buckle up. Here we go again!
©Hanna-Barbera
I’ve written about many topics over the years but nothing has ever generated as much discussion, opposition, and vitriol as challenging the cherished routine membrane sweep/stripping, aka stretch-and-sweep.
A few years ago, I wrote a post about how I’d like to see the routine, prior-to-40-weeks, without-medical-indication membrane sweep banned from obstetrical and midwifery practice. I talked about its risks and the fact that the clients I worked with called it a sexual assault when done without consent
The post went viral and I received hate messages and emails from around the world defending this procedure. In general, the sentiment was that I should most definitely be having sexual relations with myself, after which, I should be locked up and forever silenced. I also heard from hundreds of women whose births were ruined by days of painful, non-progressing contractions triggered by a membrane sweep that ended up in a fully medicalised all-the-interventions arrival for their baby that they didn’t want. And horrifically, even more hundreds wrote to share their stories of non-consenting, painful, and violating membrane sweeping when there was no reason for it, aside from the care provider’s decision that they had agency over their patient’s vagina and could do what they wanted when they wanted.
That particular post was prompted by a brief encounter with a new mother. Her baby was little and we got talking. She told me how she went to her usual prenatal visit at 36 weeks and the doctor said it was time for a vaginal check to see how things were coming along. She thought that was an ok idea and stripped accordingly, lay down on the examining table and put her feet in the stirrups. However, rather than a simple vaginal exam, she experienced excruciating pain that had her crawling up the table trying to escape that probing hand. The doctor removed her bloodied glove and when this woman asked why she was bleeding, the doctor responded, “That should get things going”. This mother had experienced a non-consenting, unplanned, and unknowing stretch-and-sweep to start labour before she or the baby were ready. She went home bleeding and cramping and within a few days went into labour and birthed a baby that was not ready to breathe. The baby spent 3 days in the NICU and she was devastated. Her birth was hijacked by a damnable routine from someone who should have known better or at least given a damn.
Yes, that was obstetrical violence. However, the routine of membrane sweeping for the mere reason that the client is at term is a deeply embedded ritual in obstetrics and mimicked by some midwives. I don’t think there is one other procedure that so callously turns a normally progressing pregnancy into a pathological event than this heinous routine.
So what is it about membrane sweeping that is so cherished that challenging it generates death threats?
Routines are habits that help organise our days
Let’s begin with some clarity on what I’m challenging.
First and foremost, I am not challenging the right for a pregnant person to choose a membrane sweep as a means of expediting labour. I fully support an individual’s right and autonomy to choose what is best for them.
Secondly, I am not challenging this as a tool for expediting labour when there is a medical indication.
I am challenging the ROUTINE of membrane sweeping that is done by some care providers as part of their normal and usual prenatal “package”, without any hint that there is a reason to expedite the birth of the baby due to an emerging medical condition.
At your cervix, ma’am
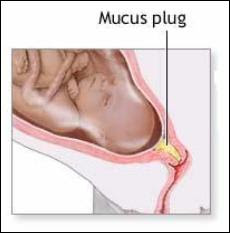
Let’s take a tour of the cervix. The cervix is a narrow passage that sits at the lower end of the uterus extending into the vagina. The cervix changes throughout the menstrual cycle and serves an important function in fertility. During ovulation, the cervix produces sperm-friendly mucus and becomes softer and more open to facilitate sperm reaching the ovum. When not ovulating, it produces sperm-unfriendly mucus and makes it more difficult for sperm to pass through to the uterus.
In pregnancy, the cervix fills with mucus, which creates a barrier to help prevent infection from passing through to the uterus. The cervix remains closed and rigid (like the tip of your nose) and is about 3-5 cm. long.
At term, in preparation for birth, the cervix will soften (like the inside of your cheek) due to the action of various hormones. The cervix is comprised of about 5-10% smooth muscle cells, which ensures it will stay closed and rigid throughout pregnancy. In preparation for labour, these muscle cells experience a programmed cellular death, which allows for the cervix to open (Leppert, 1995). The cervix will develop more oxytocin and prostaglandin receptors to help with the dilation process (Buckley, 2015). Prostaglandins, which are found abundantly in semen, ripens the cervix, digests the mucus plug, and promotes softening and shortening of the cervix.
Medical providers tend to give a great deal of attention to the cervix both prior to labour and in labour. It can provide some information that the medical folks find useful.
At term (around 40 weeks), the cervix can be felt to determine if it is ripening. Ripening means that the cervix is becoming softer, shorter, and is moving its position slightly forward. If so, it means that normal end-of-pregnancy hormones are doing their job. If not, it means that normal end-of-pregnancy hormones are doing their job, but they just haven’t gotten around to softening and shortening the cervix at the moment that a gloved hand is probing it.
This information is useful for planning an induction. A cervix that is shorter than 1.5 cm. is more predictive of spontaneous labour within the next 7-10 days than a longer cervix (Rao, Celik, Poggi, Poon, & Nicolaides, 2008). And a cervix that scores higher on the Bishop score is more predictive of an induction resulting in a vaginal birth rather than surgery (usually called “failure to progress”) (King, Pilliod, & Little, 2010). So that end-of pregnancy vaginal exam is about gathering information to plan your induction.
The other possibility for these routine (without medical indication) vaginal examinations in a healthy pregnancy is to develop submission and compliance in the client as she subjugates herself to the clinician by having her genitals penetrated by someone who is not her intimate partner.
Not too long ago, I was working with a postpartum client who was recovering from her birth experience. As a survivor of sexual assault she did not want anyone penetrating her genitals when she was labouring and giving birth and repeatedly told her midwife this. However, her midwife felt it was best for her to submit to vaginal exams in pregnancy to “get used to” them before she was in labour. Apparently, it never occurred to either of them that vaginal exams are optional and largely unnecessary for birthing a baby. In this case, the prenatal vaginal exams were for the purpose of building in submission and compliance so that the care providers could exercise agency over her body in labour.
Inductions: getting the baby out before it’s ready
An induction starts labour artificially before optimal hormonal physiology has prepared the baby and the mother for spontaneous birth. About 1 in 4 births begin by induction (BORN, 2013; Osterman & Martin, 2014). Although, there has been a slight decrease in inductions in recent years as fewer early-term inductions, meaning prior to 39 weeks, are performed. This has allowed more mothers to go into spontaneous labour without any additional adverse outcomes (Osterman & Martin, 2014). The cervix is one small part of the whole physiological process and since it can be reached easily by probing hands, it can provide a bit of information on whether an induction is likely to lead to a vaginal birth or is more likely to result in caesarean surgery.
There are lots of ways to artificially start labour before the mother or baby are ready. There are the so-called “natural” inductions:
Acupuncture and acupressure
Herbs and Homeopathy
Castor oil
Massage
Nipple stimulation
There are chemical inductions, which the literature calls “formal” inductions, as they require medical supervision:
Cervical ripening with prostaglandins
Intravenous synthetic oxytocin
And we have mechanical inductions, which also generally require medical supervision:
Artificial rupture of membranes aka “breaking the water”
Cervical ripening with a balloon catheter
Manual membrane sweeping/stripping, “stretch and sweep”
Ideally, an induction should only be suggested when the risks of staying pregnant outweigh the long and short-term risks of an induction. Depending on the method of induction those risks can include preterm birth, breathing problems in the baby, infection in the mother or baby, uterine hyper-stimulation, uterine rupture, fetal distress, breastfeeding failure, and rarely, death of either the mother or the baby.
Unfortunately, most inductions are done where the research affirms that the risks of an induction outweigh the risks of staying pregnant, including pre-labour rupture of membranes, gestational diabetes, suspected big baby, low fluid at term, isolated hypertension at term, twins, being “due”, or being “overdue” (Mozurkewich, Chilimigras, Koepke, Keeton, & King, 2009; Cohain, n.d.; Mandruzzato et al., 2010).
“membrane sweeping is a procedure meant to induce labour so that the client won’t be induced later”
Membrane sweeping: Fred Flintstone manipulating your physiology
Membrane sweeping involves the provider inserting their gloved hand into a mother’s vagina and manually stretching open the cervix and then running their finger around the opening of the cervix to separate the amniotic sack from the lower uterine segment. Caregivers will say it feels much like separating Velcro.
This procedure has the potential to trigger labour because it releases extra prostaglandins at the cervix. If the membrane sweep results in a shorter cervix, then it doesn’t make any difference in whether the mother is subsequently induced, but it does decrease the incidence of c-section. However, membrane sweeping is much more likely to result in cervical lengthening – which is predictive of NOT going into labour (Tan, Khine, Sabdin, Vallikkannu, & Sulaiman, 2011).
Prostaglandins are one of many important hormones that are needed for labour and birth. As pregnancy progresses and it’s getting time for the baby to be born, there are complex processes that prepare and protect the baby and are necessary for labour to commence. For example, the cervix and the uterus develop prostaglandin receptors so that necessary prostaglandins have a place to “land” or “connect” so that they can do their job. The uterus develops an abundance of oxytocin receptors so that this love hormone that is produced in the brain can connect with the uterus and cause contractions. The baby’s brain develops oxytocin receptors, which is neuro-protective for the journey ahead. There is an increase in estrogen, which activates the uterus for delivery. There are inflammatory processes within the uterus that help to mature the baby’s lungs to prepare for breathing on the outside. The baby’s brain develops increased epinephrine receptors to protect it from any gaps in oxygen during the birth. The mother’s brain develops endorphin receptors for natural pain relief. And there is an increase in prolactin to prepare the mother for breastfeeding and bonding. (Buckley, 2015)
When considering the finely-tuned and delicate interplay of complex and specific processes that brings the baby earth-side, a manual stretch-and-sweep at term without any medical indication is like getting Fred Flintstone to program an app that regulates the autonomic nervous system. It’s a crude, blunt instrument inserted into a complex system with the intention of bypassing evolutionarily necessary adaptive processes to cut the pregnancy short by a possible few days.
Let’s try to induce labour so we don’t have to induce labour
A Cochrane Review (Bouvain, Stan, & Irion, 2005) evaluated available studies comparing membrane sweeping to no sweeping. In general, this procedure can reduce the duration of pregnancy by up to three days. However, the authors noted that only small studies showed this reduction in pregnancy duration whereas larger studies didn’t, suggesting some bias. Because membrane sweeping doesn’t usually lead to immediate labour, it is not recommended when the need to get the baby out is urgent. Its primary use is to “prevent” a longer gestation and therefore an induction by more risky means.
A stretch-and-sweep is a procedure that is meant to induce labour so that you won’t be induced later. The Society of Obstetricians and Gynaecologists of Canada wrote in their 2013 Practice Guideline, which was reaffirmed in 2015, that “routine sweeping (stripping) of membranes promotes the onset of labour and that this simple technique decreases induction rates.”
Again: membrane sweeping is a procedure meant to induce labour so that the client won’t be induced later.
It assumes that the later induction is non-negotiable and the client’s best hope is that this early induction “saves” her from the risks of the later induction.
This is no different than all those “natural” inductions that are employed when trying to induce labour so the mother doesn’t have experience an induction – or the challenge of just declining the planned induction. It takes the approach that planned inductions are non-negotiable. Of course, mothers may chose a natural induction as a means of expediting the births of their babies for a number of reasons and I fully support their autonomy and choice to do so.
If there is a medical need to get the baby out to preserve its or its mothers life, then this dyad should be under medical supervision and receiving the best medical care possible. We need to critically evaluate the mentality that says, “let’s try to induce so we don’t have to induce”.
We’ve bought into a culture where non-evidence-based time limits and spurious reasons are given for booking inductions that don’t line up with the science. Rather than supporting mothers in exploring the science, doing a targeted risk/benefit analysis based on her particular situation, and supporting the mother in informed decision making, we line up the early inductions hoping to out-smart, out-wit, and out-play the medical providers who routinely induce based on outdated information or habit or hospital protocols that are based in their insurance risk-management strategy.
If this procedure is not recommended when there is an urgent need to get the baby out (Bouvain et al., 2005) and its primary purpose is to prevent a later induction where the indication is a pregnancy continuing beyond the cut-off date of the caregiver or institution (SOGC, 2013), then it has no medical indication.
What else did the Cochrane Review find?
There was a high level of bias in many of the studies, in part, because there could be no blinding. The clinicians knew they were performing the procedure and the clients knew they’d received it due to discomfort and pain
It was an out-patient procedure meaning there was no urgent reason for the induction
It did not generally lead to labour within 24 hours
No difference in oxytocin augmentation, use of epidural, instrumental delivery, caesarean delivery, meconium staining, admission to the NICU, or Apgar score less than seven at five minutes between sweeping and non-sweeping. This means it didn’t show any benefit
No difference in pre-labour rupture of membranes, maternal infection or neonatal infection. However, it’s worth noting that the non-sweeping participants were subject to routine obstetrical services that includes many vaginal exams that increase pre-labour rupture of membranes and infection (Maharaj, 2007; Zanella et al., 2010; Lenihan, 1984; Critchfield et al., 2013)
Significant pain in the mother during the procedure
Vaginal bleeding after the procedure
Painful contractions for the next 24 hours not leading to labour
What we have here is a routine that hurts the mother and has no significant benefit – aside from maybe possibly putting her into labour before another planned induction.
As the Cochrane Review discovered, the likely outcome of a membrane sweep is painful non-progressing contractions. This is often mis-interpreted as “labour” and the client is sent to the hospital for an induction anyway because she’s been “in labour” for 24-48 hours without progress. This is the epitome of a hijacked birth that turns a normal physiological process into a pathological one leading to the cascade of interventions, sometimes all the way up to an unwanted and unplanned caesarean for “failure to progress”. To convert the natural process into a pathological one is part of the classic definition of obstetrical violence (D'Gregorio, 2010).
They call it ‘birth rape’
For those who experienced this without their prior knowledge or consent, their comments overwhelmingly spoke of rape. This was especially pronounced in those with a history of prior rape. Studies confirm that those with a history of rape experience the routines of industrial birth differently than those without a history of sexual assault. For survivors, procedures that are uneventful for others can inadvertently put them “back in the rape” (Halvorsen, Nerum, Øian, & Sørlie, 2013).
Frankly, it’s unconscionable that any care provider would brazenly take the opportunity to manually manipulate a woman’s cervix, knowing it introduces risks and has the potential to hurt her, without the express knowledge and consent of the client following an informed choice discussion.
While membrane sweeping is intended to induce labour, it’s also used on labouring women to hurry things along. During labour, the cervix is being moved and thinned by the action of uterine muscles contracting and pulling the cervix up and around the baby’s head. The cervix is working hard and it’s tender. Many women will report that they screamed, cried ‘no’, tried to kick the provider’s hand away, or tried to crawl up the bed to get away from the invasive exam.
I remember one dark cold February night, years ago, when I was called to be with a family in labour. There was an ice storm and my trip there was dangerous and precarious. Eventually, my car slid into their street and managed to stop somewhere close to the driveway. I quietly entered the house to hear a mother in the throes of glorious, deep, active labour. I knew it wouldn’t be long before the baby arrived. I announced myself and tiptoed upstairs to see her on hands and knees with more blood than I would have expected on the towel beneath her. She said she invited her midwife to the birth and expected her to be there any minute. Soon enough, a beautiful baby boy gently emerged and landed safely into his daddy’s waiting hands. By the time the midwives arrived, the new family was tucked into bed enjoying a post-birth snack and cup of tea.
As the new family was bonding, I joined the midwives downstairs who were making notes in their client’s medical charts to make them some tea and offer a snack. I overheard one midwife say, “Oh yeah, when I was here earlier, she was about 6cm so I did a stretch-and-sweep”.
“Oh yeah.
Now I remember.
She was in active labour so I did an invasive and painful procedure to speed things up during a dark and dangerous ice storm.
Without her knowing I would do that.”
This is nothing but reckless cruelty. Yet this kind of cruelty permeates maternity services where women are routinely hurt for the sole purpose of interfering in their physiology and the safety of the birth process in order to get the baby out before they do even more risky and dangerous things.
And that is why I would like to see the ROUTINE, WITHOUT MEDICAL INDICATION membrane sweep removed from obstetrical and midwifery practice. It shouldn’t be the luck of the draw that a pregnant client gets one of the “good ones” who only induces a client when there is a medical need, with an informed choice discussion, and full consent.
To return to my original question: what is it about membrane sweeping that is so cherished that challenging it generates death threats?
It’s a deeply embedded ritual in a toxic medical culture that presumes to take authority over a pregnant woman’s sexual organs for the purpose of dominating the physiological process and then becoming a hero to the interrupted physiology and complications that ensue. It’s about power and control. And challenging this is a dangerous act of sedition. Those who do this to their clients like being the hero and clients who defend this need to believe they were saved from something – otherwise the truth is just too awful.
Make wise choices.
Much love,
Mother Billie
#endobstetricalnonsense #informedconsent #obstetricalviolence #membranesweeping #stretchandsweep #withoutconsent #birthrape #failuretoprogress
References
Better Outcomes Registry Network. (BORN). 2013. Provincial Overview of Perinatal Health in 2011–2012.
Boulvain, M., Stan, C. M., & Irion, O. (2005). Membrane sweeping for induction of labour. Cochrane Database of Systematic Reviews, (1).
Buckley, S. J. (2015). Hormonal physiology of childbearing: Evidence and implications for women, babies, and maternity care. Washington, DC: Childbirth Connection Programs, National Partnership for Women & Families.
Cohain, J. S. Reducing Inductions: Lack of Justification to Induce for “Postdates”.
Critchfield, A. S., Yao, G., Jaishankar, A., Friedlander, R. S., Lieleg, O., Doyle, P. S., ... & Ribbeck, K. (2013). Cervical mucus properties stratify risk for preterm birth. PloS one, 8(8), e69528.
D'Gregorio, R. P. (2010). Obstetric violence: a new legal term introduced in Venezuela.
Halvorsen, L., Nerum, H., Øian, P., & Sørlie, T. (2013). Giving birth with rape in one's past: a qualitative study. Birth, 40(3), 182-191.
King, V., Pilliod, R., & Little, A. (2010). Rapid review: Elective induction of labor. Portland: Center for Evidence-based Policy.
Lenihan, J. J. (1984). Relationship of antepartum pelvic examinations to premature rupture of the membranes. Obstetrics and gynecology, 63(1), 33-37.
Leppert, P. C. (1995). Anatomy and physiology of cervical ripening. Clinical obstetrics and gynecology, 38(2), 267-279.
Maharaj, D. (2007). Puerperal pyrexia: a review. Part II. Obstetrical & gynecological survey, 62(6), 400-406.
Mandruzzato, G., Alfirevic, Z., Chervenak, F., Gruenebaum, A., Heimstad, R., Heinonen, S., ... & Thilaganathan, B. (2010). Guidelines for the management of postterm pregnancy. Journal of perinatal medicine, 38(2), 111-119.
Mozurkewich, E., Chilimigras, J., Koepke, E., Keeton, K., & King, V. J. (2009). Indications for induction of labour: a best‐evidence review. BJOG: An International Journal of Obstetrics & Gynaecology, 116(5), 626-636.
Osterman, M. J., & Martin, J. A. (2014). Recent declines in induction of labor by gestational age.
Rao, A., Celik, E., Poggi, S., Poon, L., & Nicolaides, K. H. (2008). Cervical length and maternal factors in expectantly managed prolonged pregnancy: prediction of onset of labor and mode of delivery. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, 32(5), 646-65.
Rayburn, W. F., & Zhang, J. (2002). Rising rates of labor induction: present concerns and future strategies. Obstetrics & gynecology, 100(1), 164-167.
Society of Obstetricians and Gynaecologists of Canada. SOGC. 2013. Clinical Practice Guideline, No. 296, Indution of Labour.
Tan, P. C., Khine, P. P., Sabdin, N. H., Vallikkannu, N., & Sulaiman, S. (2011). Effect of membrane sweeping on cervical length by transvaginal ultrasonography and impact of cervical shortening on cesarean delivery. Journal of Ultrasound in Medicine, 30(2), 227-233.
Zanella, P., Bogana, G., Ciullo, R., Zambon, A., Serena, A., & Albertin, M. A. (2010). Chorioamnionitis in the delivery room. Minerva pediatrica, 62(3 Suppl 1), 151-153.
Hocus Pocus - The ARRIVE study says inductions reduce caesareans
In an epic sleight of hand, the US obstetrical industry has managed to produce a study that affirms the “benefits” of universal elective induction of labour at 39 weeks. Headlines have trumpeted this remarkable accomplishment! Inducing labour early “prevents” c-sections!
The conclusion of the much anticipated ARRIVE study are presented in their abstract:
“IOL (induction of labour) in low-risk nulliparous women (first-time mothers) results in a lower frequency of CD (caesarean delivery) without a statistically significant change in the frequency of a composite of adverse perinatal outcomes.”
Obstetricians now have the much-desired go-ahead to routinely induce healthy first-time mothers prior to reaching 40 weeks under the guise that it will reduce c-sections with no additional negative outcomes to the mother or baby.
This is the same outrageous chicanery that brought us the ridiculously executed Term Breech Trial that changed obstetrical practices around the world. It was the excuse the industry was looking for to do what they already wanted to do: surgery.
In an epic sleight of hand, the US obstetrical industry has managed to produce a study that affirms the “benefits” of universal elective induction of labour at 39 weeks. Headlines have trumpeted this remarkable accomplishment! Inducing labour early “prevents” c-sections!
The conclusion of the much anticipated ARRIVE study (Grobman et al., 2018) are presented in their abstract:
“IOL (induction of labour) in low-risk nulliparous women (first-time mothers) results in a lower frequency of CD (caesarean delivery) without a statistically significant change in the frequency of a composite of adverse perinatal outcomes.”
Obstetricians now have the much-desired go-ahead to routinely induce healthy first-time mothers prior to reaching 40 weeks under the guise that it will reduce c-sections with no additional negative outcomes to the mother or baby.
This is the same outrageous chicanery that brought us the ridiculously executed Term Breech Trial that changed obstetrical practices around the world (Hannah et al., 2000). It was the excuse the industry was looking for to do what they already wanted to do: surgery (Hunter, 2013).
Obstetrics is a surgical speciality that also includes attending normal physiologic births. Years ago, the World Health Organisation sought to address disparities in health outcomes around the world in an effort to reduce maternal deaths in vulnerable places. They looked at countries with good outcomes and compared them to countries with poor outcomes. In wealthy nations where infrastructure was in place, food was easily accessible, and infection control measures were widely used, they tended to have a c-section rate around 5%. The WHO initially suggested that a c-section rate of 5-10% across the entire population could improve maternal-fetal outcomes. However, when the c-section rate rose above 15% across a population, the maternal death rate began to rise due to too much surgery.
There was naturally an outcry from the wealthy sector that was safely performing a lot of surgery and the WHO was roundly chastised for trying to prevent them from performing surgery on clients whom they believed would benefit from surgery. So the WHO said a c-section rate of 10-15% was “ideal” as it could potentially save lives, although they’ve subsequently stated that there is no benefit when the rate rises about 10% for a population (Betran, Torloni, et al, 2016).
Caesarean rates by country. (Betran, Ye, et al, 2016)
The problem wasn’t lack of surgery. The problem was that 99% of maternal deaths are in the developing world with half in sub-Sahara Africa and one-third in Southeast Asia where most fatal complications develop during pregnancy and are largely preventable or treatable. Half of these maternal deaths occur in fragile and humanitarian settings such as refugee displacement, natural disasters, and war (WHO, 2018).
Since the WHO’s mistake in encouraging an increase in surgery in impoverished, fragile, and humanitarian settings, the rest of the world’s obstetrics industry has spiraled out of control. Canada’s national c-section rate has risen to 28.2% in 2016-17 (CIHI, 2018) along with an increase in most every other country.
Data from around the world shows an average annual rate of increase in caesarean surgery of 4.4% from 1990 to 2014 (Betran, Ye, et al, 2016). Globally, in 2015 21.1% of all births occur through caesarean surgery, representing just over one in five mothers around the world (Boerma et al., 2018). This rate has risen from 12.1% of all births in 2000, representing a relative increase of 74.38% in just 15 years.
Regionally, caesarean rates are:
Latin America & Caribbean: 44.3% - an absolute increase of 19.4% and a relative increase of 77.91% (from 24.9% to 44.3%)
North America: 32.3% - an absolute increase of 10% and a relative increase of 44.84% (from 22.3% - 32.3%)
Oceania: 32.6% - an absolute increase of 14.1% and a relative increase of 76.22% (from 18.5% to 32.6%)
Europe: 27.3% - an absolute increase of 16.1% and a relative increase of 143.75% (from 11.2% to 27.3%)
Asia: 19.2% - an absolute increase of 15.1% and a relative increase of 343.18% (from 4.4% to 19.5%)
Africa: 7.3% - an absolute increase of 4.5% and a relative increase of 155.17% (from 2.9% to 7.4%)
Global increase in caesarean surgery 1990-2014. (Betran, Ye, et al, 2016)
What’s to blame for these shocking numbers? While it’s common to say it’s due to older, heavier, or more unhealthy mothers, the truth is that caesarean surgery has risen for every clientele group including young, slim, and healthy mothers.
The real increase in surgery comes from:
The management style of the hospital, where proactive management of patient flow and nursing resources results in more surgery and more postpartum haemorrhages (Plough et al., 2017)
Fear of litigation, particularly when malpractice premiums rise about $100,000 (Zwecker, Azoulay, & Abenhaim, 2011)
Financial incentives. Private facilities tend to perform more surgery as their clients have private insurance to pay for it (Dahlen et al., 2012). Even in the Canadian system, where compensation comes from a single payer through universal coverage, when the compensation for surgery is double that of a vaginal delivery, then there is a corresponding 5.6% increase in surgery when all else is equal (Allin, Baker, Isabelle, & Stabile, 2015)
Training, scheduling, and institutional culture drive the rates of surgery in individual institutions (Roth & Henley, 2012)
Both maternal request and maternal morbidity has been blamed for the dramatic increase in surgery, but neither has held up to scrutiny. The increase is physician induced (Roth & Henley, 2012).
Tomasz Kobosz freeimages.com
Now this same industry that has brought us shockingly high rates of surgery due to the nature of the industry says they have a “solution” for this epidemic: induce healthy mothers early.
The caesarean epidemic is due to the industry wanting to perform surgery. The unsupportable conclusions of the Term Breech Trial turned the industry upside-down in a heartbeat and most mothers with a breech-presenting baby are now faced with mandatory surgery. This industry is so invested in getting their way that some of their members have even resorted to using the courts to force clients into non-consenting procedures (Diaz-Tello, 2016).
The idea that inducing a mother early will reduce the incidence of caesarean surgery is akin to saying that if you give a child a pre-dinner snack then they are less likely to over-eat at dinner. Fulfilling the need to medically manage the client’s physiology satisfies the surgeon’s training, preferences, and institutional culture that guide the physician to perform surgery. This is nothing more than a physician placebo. And when this pre-dinner snack doesn’t satisfy any more, and the honeymoon phase of routine early induction wanes, then rates of surgery will rebound.
To begin, an induction is not benign. The risks associated with an induction depend on what is done to the patient. This could involve multiple vaginal exams (infection, sexual re-traumatisation), artificial rupture of membranes (cord prolapse, infection, foetal distress), continuous foetal monitoring (caesarean surgery), chemical cervical ripening (uterine hyperstimulation, uterine rupture, foetal distress, maternal death, foetal death, meconium), IV synthetic oxytocin (Pitocin/syntocinon) (uterine rupture, postpartum haemorrhage, breastfeeding failure, postpartum depression and anxiety, water intoxication leading to convulsions, coma or death, foetal distress, meconium, neonatal jaundice, neonatal brain damage, and neurological dysregulation in the child years later) (Gregory, Anthopolos, Osgood, Grotegut, & Miranda, 2013; Grotegut, Paglia, Johnson, Thames, & James, 2011; Gu et al., 2016; Kurth & Haussmann, 2011; Elkamil et al., 2011).
Inductions are generally more painful and first time mothers are more than 3x more likely to ask for an epidural during an induction (Selo-Ojeme et al., 2011). This leads to a longer labour and pushing stage, need for more synthetic oxytocin, problems passing urine, inability to move after the birth, fever, and more instrumental deliveries (Anim-Somuah, Smyth, Cyna, & Cuthbert, 2018).
Now let’s talk about the study itself.
A total of 3062 women were assigned to labour induction, and 3044 were assigned to expectant management (wait and see approach). Just like with the Term Breech Trial, there was quite a bit of crossover, meaning those who were assigned to the induction group had a spontaneous birth and those who were assigned to a wait-and-see approach were induced (about 5% from each group – 1 in 20 participants). However, the results were reported to the group they were assigned to.
The enrolment was designed to be too small to detect certain outcomes. Adverse outcomes such as maternal death, cardiac arrest, anaesthetic complications, thromboembolism, amniotic fluid embolism, major puerperal infection, or haemorrhage are fairly rare but are associated with both induction and surgery.
Without enough participants, it’s not possible to determine if there was an increase in adverse outcomes from inducing mothers.
Remember, this study took place in the US where they boast some of the worst maternal and neonatal outcomes in the developed world. How they practice obstetrics has much to do with this. Both the induction and the expectant management groups experienced high rates of interventions and the outcomes for the babies were consistent with that:
15% were not breathing at all or were breathing weakly 5 minutes after birth
12% were admitted to the NICU
5% had neonatal jaundice
1% needed breathing support for a day or more
0.7% experienced meconium aspiration syndrome
0.6% had hypoxic ischemic encephalopathy
0.3% suffered intracranial haemorrhage
0.3% had infections
0.2% had seizures
The results for the mothers were equally awful:
5% had severe postpartum haemorrhage of over 1500cc requiring a blood transfusion, blood products, or a hysterectomy
4% suffered a third or fourth degree perineal tear
2% had a postpartum infection
Benjamin Earwicker freeimages.com
With shockingly terrible results like this, the industry has the temerity to suggest that signing up for an elective induction to placate their nerves is a good idea because they’re less likely to perform surgery?
Frankly, it’s asinine nonsense from a group that needs a dramatic change in education and culture. We’ll see how long it takes for this insanity to move throughout the obstetrical world.
Make wise choices, my friends.
Much love,
Mother Billie
References
Allin, S., Baker, M., Isabelle, M., & Stabile, M. (2015). Physician Incentives and the Rise in C-sections: Evidence from Canada (No. w21022). National Bureau of Economic Research.
Anim-Somuah, M., Smyth, R. M., Cyna, A. M., & Cuthbert, A. (2018). Epidural versus non-epidural or no analgesia for pain management in labour. The Cochrane database of systematic reviews, 5, CD000331-CD000331.
Betrán, A. P., Torloni, M. R., Zhang, J. J., Gülmezoglu, A. M., WHO Working Group on Caesarean Section, Aleem, H. A., ... & Deneux‐Tharaux, C. (2016). WHO Statement on caesarean section rates. BJOG: An International Journal of Obstetrics & Gynaecology, 123(5), 667-670.
Betrán, A. P., Ye, J., Moller, A. B., Zhang, J., Gülmezoglu, A. M., & Torloni, M. R. (2016). The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PloS one, 11(2), e0148343.
Boerma, T., Ronsmans, C., Melesse, D., Barros, A., Barros, F., Juan, L., Moller, A., Say, L., Hosseinpoor, A., Mu, Y., Neto., D., Temmerman, M. (2018). Global epidemiology and use of and disparities in caesarean section. The Lancet. Volume 392, Issue 10155, P1341-1348, October 12, 2018.
CIHI. Canadian Institute for Health Information. (2018). Hospital Morbidity Database, 2016–2017.
Dahlen, H. G., Tracy, S., Tracy, M., Bisits, A., Brown, C., & Thornton, C. (2012). Rates of obstetric intervention among low-risk women giving birth in private and public hospitals in NSW: a population-based descriptive study. BMJ open, 2(5), e001723.
Diaz-Tello, F. (2016). Invisible wounds: obstetric violence in the United States. Reproductive Health Matters.
Elkamil, A. I., Andersen, G. L., Salvesen, K. Å., Skranes, J., Irgens, L. M., & Vik, T. (2011). Induction of labor and cerebral palsy: a population‐based study in Norway. Acta obstetricia et gynecologica Scandinavica, 90(1), 83-91.
Gommers, J. S., Diederen, M., Wilkinson, C., Turnbull, D., & Mol, B. W. (2017). Risk of maternal, fetal and neonatal complications associated with the use of the transcervical balloon catheter in induction of labour: A systematic review. European Journal of Obstetrics & Gynecology and Reproductive Biology, 218, 73-84.
Gregory, S. G., Anthopolos, R., Osgood, C. E., Grotegut, C. A., & Miranda, M. L. (2013). Association of autism with induced or augmented childbirth in North Carolina Birth Record (1990-1998) and Education Research (1997-2007) databases. JAMA pediatrics, 167(10), 959-966.
Grotegut, C. A., Paglia, M. J., Johnson, L. N., Thames, B., & James, A. H. (2011). Oxytocin exposure during labor among women with postpartum hemorrhage secondary to uterine atony. American journal of obstetrics and gynecology, 204(1), 56-e1.
Grobman, W. A., Rice, M. M., Reddy, U. M., Tita, A. T., Silver, R. M., Mallett, G., ... & Rouse, D. J. (2018). Labor induction versus expectant management in low-risk nulliparous women. New England Journal of Medicine, 379(6), 513-523.
Gu, V., Feeley, N., Gold, I., Hayton, B., Robins, S., Mackinnon, A., ... & Zelkowitz, P. (2016). Intrapartum synthetic oxytocin and its effects on maternal well‐being at 2 months postpartum. Birth, 43(1), 28-35.
Hannah, M. E., Hannah, W. J., Hewson, S. A., Hodnett, E. D., Saigal, S., Willan, A. R., & Collaborative, T. B. T. (2000). Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. The Lancet, 356(9239), 1375-1383.
Hunter, B. (2013). Implementing research evidence into practice: some reflections on the challenges. Evidence based midwifery, 11(3), 76-80.
Kurth, L., & Haussmann, R. (2011). Perinatal Pitocin as an early ADHD biomarker: neurodevelopmental risk?. Journal of attention disorders, 15(5), 423-431.
Linton, A., Peterson, M. R., & Williams, T. V. (2004). Effects of maternal characteristics on cesarean delivery rates among US Department of Defense healthcare beneficiaries, 1996–2002. Birth, 31(1), 3-11.
Plough, A. C., Galvin, G., Li, Z., Lipsitz, S. R., Alidina, S., Henrich, N. J., ... & McDonald, R. (2017). Relationship between labor and delivery unit management practices and maternal outcomes. Obstetrics & Gynecology, 130(2), 358-365.
Roth, L. M., & Henley, M. M. (2012). Unequal motherhood: racial-ethnic and socioeconomic disparities in cesarean sections in the United States. Social Problems, 59(2), 207-227.
Selo-Ojeme, D., Rogers, C., Mohanty, A., Zaidi, N., Villar, R., & Shangaris, P. (2011). Is induced labour in the nullipara associated with more maternal and perinatal morbidity?. Archives of gynecology and obstetrics, 284(2), 337-341.
Washington, S., Caughey, A. B., Cheng, Y. W., & Bryant, A. S. (2012). Racial and ethnic differences in indication for primary cesarean delivery at term: experience at one US Institution. Birth, 39(2), 128-134.
WHO, World Health Organization. (2018). Fact Sheet-Maternal Mortality.
Zwecker, P., Azoulay, L., & Abenhaim, H. A. (2011). Effect of fear of litigation on obstetric care: a nationwide analysis on obstetric practice. American journal of perinatology, 28(04), 277-284.
Me too
Recently, #metoo went viral as hundreds of thousands of women, and some men, said “me, too, I’ve been sexually harassed, assaulted or violated”. There were stories told for the first time. There were experiences re-told through a stronger voice. And in private forums, women told of rapes, childhood molestation, being drugged, and more. Some couldn’t post “me too” on their social media stories because they didn’t want their parents to know, believed they were partly to blame, or felt it was too exposing. One woman said she didn’t want the world to know she was “weak”. When asked, she said she wasn’t strong enough to fight off her attacker and she felt ashamed for it.
There were waves of trauma as some survivors found it too overwhelming to see the hundreds of #metoo’s across their news feeds and had to disconnect until it passed. It was not comforting to know they were not alone. It was horrifying.
And this isn’t just an issue of female looking or female identifying individuals being sexually violated. Men and boys are also sexually assaulted. Yet, from a cultural perspective, the response is different. Males are not told that “boys will be boys” or "girls will be girls" and they just normally like to grope and grab and hump and fondle males. Males are rarely depicted being sexually assaulted in music videos as a form of entertainment. They are not routinely asked what they were wearing, if they were out alone, if they went to a party, or if they were drinking. As a culture, we don’t victim blame males to the same extent that we victim blame females.
“You know sexual violence knows no race or color or gender or class. But the response to sexual violence does.” ~ Tarana Burke
Tarana Burke began the “me too” campaign in 2006 as a means of helping women who had been sexually assaulted not feel so alone. It was meant especially for girls and women of colour who had survived sexual violence to inspire empowerment through empathy. It was not only “to show the world how widespread and pervasive sexual violence is, but also to let other survivors know they are not alone.”
Recently, #metoo went viral as hundreds of thousands of women, and some men, said “me, too, I’ve been sexually harassed, assaulted or violated”. There were stories told for the first time. There were experiences re-told through a stronger voice. And in private forums, women told of rapes, childhood molestation, being drugged, and more. Some couldn’t post “me too” on their social media stories because they didn’t want their parents to know, believed they were partly to blame, or felt it was too exposing. One woman said she didn’t want the world to know she was “weak”. When asked, she said she wasn’t strong enough to fight off her attacker and she felt ashamed for it.
There were waves of trauma as some survivors found it too overwhelming to see the hundreds of #metoo’s across their news feeds and had to disconnect until it passed. It was not comforting to know they were not alone. It was horrifying.
And this isn’t just an issue of female looking or female identifying individuals being sexually violated. Men and boys are also sexually assaulted. Yet, from a cultural perspective, the response is different. Males are not told that “boys will be boys” or "girls will be girls" and they just normally like to grope and grab and hump and fondle males. Males are rarely depicted being sexually assaulted in music videos as a form of entertainment. They are not routinely asked what they were wearing, if they were out alone, if they went to a party, or if they were drinking. As a culture, we don’t victim blame males to the same extent that we victim blame females.
Unfortunately, as a group, female looking individuals beyond a certain age have almost universally been subjected to sexual objectification, harassment, violation or assault. And the problem is not that they are female looking, but that as a culture, we condone violence against them.
“Rape culture” is a term that describes a society that normalises sexual violence. Rape culture is perpetuated through the use of misogynistic language, the objectification of women’s bodies, and the glamorization of sexual violence, to the point where society disregards women’s rights and safety.
Sexual violence exists along a continuum that ranges from sexual remarks to sexual touching to rape. In a rape culture, both men and women assume that sexual violence is a fact of life. Rape culture includes jokes, TV, music, advertising, words, imagery and laws that make violence against women and sexual coercion seem so normal that people believe that it’s inevitable.
What does this do to women as they access health care services?
Some are keenly aware that they receive breast and pelvic examinations when there’s no logical reason for them. And some doctors will admit to getting some sexual gratification from performing these procedures. Yet, despite any ‘warning bells’ or intuition, women are told that any physical investigation by anyone with a medical licence is for their own good and is wholly benign and acceptable. Outside of medicine, we call this gaslighting.
Gaslighting is a form of manipulation where the individual is repeatedly told that their experience and their perceptions are wrong in order to cause the victim to doubt her or himself, and ultimately lose her or his own sense of perception, identity, and self-worth.
The annual pelvic exam (not the same thing as a pap test) is no longer recommended for asymptomatic women by the American College of Physicians, as a review of 70 year’s worth of studies shows it has no benefit in terms of detecting ovarian cancer, nor reducing deaths from ovarian cancer. It does, however, cause distress for more than one third of women who received these exams where survivors of sexual assault were more likely to find them painful, embarrassing and upsetting.
Yet despite the annual pelvic exam having no benefits for asymptomatic females and not being an evidence based procedure, ACOG remained firm that it was part of the “well-woman visit” that helped to establish “open communication”. It’s curious how having a provider’s hand inside a woman’s vagina, causing her embarrassment and discomfort, establishes open communication. It seems that she is expected to strip, lie down, spread her legs and take it. And this is her being a good girl, a good patient, and open to “communication” with her provider. Again, outside of medicine, we call this gaslighting.
For survivors of sexual abuse, the routine gynaecologic exam can provoke more intensely negative feelings including more trauma-like responses during the examination. This includes intrusive or unwanted thoughts, memories, body memories and feelings of detachment from their bodies. This is what is termed “re-experiencing”. Some survivors re-experience the sensations and memories of their sexual abuse during routine gynaecologic procedures (Robohm & Buttenheim, 1997).
Still, it’s normal for survivors to be told that the pelvic exam is nothing like their assault, and that they are out of their minds for even suggesting it. Comments on social media can take a quick turn to outrage that the provider isn’t a sexual abuser (even if he is - see below), thus derailing the conversation, which was to illuminate the survivor’s experience and then eventually to engage in a discussion about appropriate trauma informed clinical services. Again, it’s gaslighting to accuse the survivor who speaks of her personal experience of either saying the experience was not abusive when it was or of saying the clinician was the abuser when she is speaking of a memory or a flashback. The survivor is perfectly capable of distinguishing an assault from a memory. This manipulation is to ensure survivors are not to believe their sensations and perceptions and that no one else will believe them either. They are not to trust themselves but only what they are told.
Fortunately, most providers engage in sensitive and evidence based interactions with their clients. Given the high likelihood that most women have been the victim of sexual suggestion, objectification, discrimination, harassment, molestation, assault or rape, there are guidelines to help a clinician conduct a sensitive examination along with the assurance that the examination will stop when the client tells them to (Bates, Carroll, & Potter, 2011).
The doctor’s office is quite adaptive to trauma informed services for survivors, and in fact, might be the one place where the victim feels safe to reveal her history. The labour and delivery ward, however, can be highly problematic.
Modern institutional maternity services are designed to run with cost-and-time effective efficiency. Labour and delivery units have been modeled after Henry Ford’s manufacturing conveyor belt to ensure quick, efficient and uniform production and services (Perkins 2004). There are time limits (aka Friedman’s Curve) for each stage of labour where an intervention to speed things up helps to manage resources. Routines that have no benefit for the mother or baby (continuous electronic fetal monitoring, admission non-stress test) are applied as a means of lessening the potential for litigation while also introducing the potential for misdiagnosis and further interventions (Clarke, 2015).
The psychological aftermath of sexual assault, fear, anxiety, depression, fatigue, chronic pain, sleep or eating disturbances, self-harm, substance abuse and suicidal thoughts or attempts, have been termed Rape Trauma Syndrome (RTS). Those who suffer from Rape Trauma Syndrome have more serious symptoms than individuals who develop PTSD from other stressors. The closer the assault is to the legal definition of rape, forced and non-consenting sexual activity, the more intense the symptoms of RTS (Faravelli, Giugni, Salvatori, & Ricca, 2004).
Does a woman’s prior sexual abuse affect her experience of her provider’s services in birth? It can.
In interviewing mothers who had been raped and then gave birth, either vaginally or surgically, participants were given the opportunity to expand on their experience. As their narratives were analysed, the primary theme that emerged was that they experienced it as “being back in the rape” (Halvorsen, Nerum, Øian, & Sørlie, 2013).
During birth, their memories of their rape included:
Lying supine, forcibly restrained
Violent approach to the body/genitals
Painfully forced entry and vaginal penetration
Perpetrator takes over control of her body
Struggle, shouting, crying for help
Darkness, blood, semen, sweat, breath
Feels unclothed, despised
Helpless, degraded,
Gives up, lets it happen, feels ashamed, leaves her body, disappears
The triggers for these memories of their rape came from the routine conditions of their birth experience:
Being placed supine, physically restrained
Legs forced apart, placed in stirrups
Invasive procedures, not being listened to or seen
Invasive vaginal examinations
Unfamiliar hands touching body, being overruled
Sight/smell of blood, amniotic fluid, feces, sweat
Dimmed lighting/being unclothed
Bodily integrity not ensured
Being tied to bed or operating table, giving up
Birth attendants control body, room, time
In reflecting on this study, it’s not hard to understand why some women use the expression “birth rape”. Their births felt like a rape (Reed, Sharman, & Inglis, 2017).
For a mother who has been sexually assaulted, she may not experience the routines of birth, such as cervical exams, as benign. To her they may be sexually violating, particularly when the birth attendants don’t take the time to discuss the routines with her, ask her for her permission, wait for her to consent and then accept her refusal should she decline.
A critical issue in maternity services, as defined by the clients, is that maternal autonomy and consent are still nebulous concepts for many operators in the industry. In a survey of over 1500 doulas in the US and Canada (Roth et al., 2014),
71.2% had witnessed a care provider pull the dead baby card, i.e., tell a client that her baby might die if she didn’t agree to a proposed procedure
88.6% had witnessed a care provider engage in a procedure without giving the client a choice or time to consider the procedure
58.7% had witnessed a care provider engage in a procedure explicitly against the wishes of the client
The closer the assault is to the legal definition of rape, forced and non-consenting sexual activity, the more intense the symptoms of RTS (Faravelli et al., 2004). A woman who experiences her birth as forced and non-consenting sexual activity is at profound risk of negative physical, emotional, psychological and relational consequences.
#metoo happens in birth as well.
This isn’t to vilify individual providers within the maternity industry. It’s a cultural issue that is deep and complex. The hospital is a microcosm of the society in which it exists (Bowser & Hill, 2010). It is not set up to support clients who have already been subject to sexual violation. Just as much of society is not equipped to engage with their female members as equal partners.
In some hospitals, the client may choose to declare her past and set up an appointment with the hospital social worker to come up with a plan for respectful care that includes protecting her dignity, obtaining her consent and engaging in trauma informed care. Given how few individuals report sexual violations, it’s hard to have much faith in this approach. This depends on the victim declaring herself vulnerable in order to modify the behaviour of the staff. Is the client who does not expose her previous violations not afforded the same concessions of dignity, consent and trauma informed care?
And it’s not just hospitals where survivors are fighting to have their dignity and their rights respected. Home birth clients who have engaged a midwife can also experience the same difficulties in ensuring an appropriate trauma informed approach. A pregnant mother planning a home birth contacted Birth Trauma Ontario with this message: "I'm 37+3 and I met with my midwives this morning and they would like to terminate our relationship because they are concerned about the tone of my birth plan and feel that I am placing my baby in danger by declining routine pelvic exams during labour. What the f*ck do I do?" The mother was open to checks if there is a reason but didn't want regular exams every few hours. The midwife terminated their relationship shortly after her client sent this message.
When birthing clients register complaints about procedures done unnecessarily or without consent or after consent was removed, the typical response from the hospital or the regulatory body is that she didn’t understand what happened to her. She's told her provider was saving hers and her baby’s life. And she ought to be grateful. It’s one of the supremest forms of gaslighting and birthing women experience it all the time. Even in general society, when a mother talks about how difficult or traumatic her birth was or that her wishes were disregarded, the usual response is that she should be grateful, as the baby is all that matters. Somehow, we think babies can thrive with broken mothers if they just ignore their own needs enough.
Giving birth is pretty much the same, physiologically speaking, across most mammals, including humans. However, how we do birth is wholly cultural. In this culture of #metoo, women are expected to submit to routines and procedures that expose them, frighten them, penetrate them, and rob them of their dignity because it’s what women do to have a baby. Asking for a better experience is called selfish.
Rape culture affects all of us and it’s pervaded the delivery room where men sometimes still “joke” about a “husband stitch” to make her perineum nice and tight for the pleasure of the penis that will penetrate her after her recovery. Where women are still forced to birth on their backs in order to accommodate the skills limitations of the paid provider. Where strangers come and go. Where she receives routine cervical checks that are primarily for the benefit of the institution’s time and resource management. Where she is given no choice regarding the birth of her breech baby. Where she still hears providers pull the dead baby card in order to gain her compliance.
When Tarana Burke talks about how #metoo has gone viral, she is concerned whether those who helped to inspire women to disclose their stories of survival are prepared for what comes next.
There are many of us who are prepared. We understand that sexual violation writes on the fabric of who you are. We know that you sometimes want more time to choose your path – for birth and beyond without arbitrary time limits. We know that you don’t trust everyone, including yourself at times. We know that you have been manipulated and need to know that no one will use manipulation or coercion to gain your compliance. We know that you don’t want to be insulted by being told to stay off the internet. We understand that safety is more than a baby who is alive at the end of the process. It’s also about whether your spirit and your soul are alive as well. We know that you have requirements for your dignity and they may not be the same as your neighbour’s. We know that you don’t respect threats, lies or coercion. We know that if there’s going to be a power imbalance in the relationship, then you are the one with the power. We ask you for your truth as that’s more relevant that a practice guideline or a study.
As individuals are still reeling from the massive participation and revelation in the #metoo campaign, this is a good time to consider how we treat each other when it comes to personal boundaries and intimacy. Pregnancy, birth, and breastfeeding are deeply personal and intimate experiences. It’s time to take a good look at our rape culture for what it is and to begin to connect with birthing clients in a way that honours each one’s dignity, experiences and boundaries. We need to work together to ensure birthing families have real choices that respect their history, their values, their future, their hopes and their identity.
And for every person who said #metoo, there are hundreds and thousands more who didn’t say it but have experienced it nonetheless. Let’s be kind together and help each other heal. And let’s help each other to experience birth in a new culture of love and respect. Let’s learn the art of trauma informed care and learn to ask better questions and to offer options that really support each other. Together we are stronger.
Much love,
Mother Billie
References
Bates, C. K., Carroll, N., & Potter, J. (2011). The challenging pelvic examination. Journal of general internal medicine, 26(6), 651-657.
Bowser, D., & Hill, K. (2010). Exploring evidence for disrespect and abuse in facility-based childbirth. Boston: USAID-TRAction Project, Harvard School of Public Health
Clarke, E. (2015). Law and Ethics for Midwifery. Routledge.
Faravelli, C., Giugni, A., Salvatori, S., & Ricca, V. (2004). Psychopathology after rape. American Journal of Psychiatry, 161(8), 1483-1485.
Perkins, B. B. (2004). The medical delivery business: Health reform, childbirth, and the economic order. Rutgers University Press.
Halvorsen, L., Nerum, H., Øian, P., & Sørlie, T. (2013). Giving birth with rape in one's past: a qualitative study. Birth, 40(3), 182-191.
Reed, R., Sharman, R., & Inglis, C. (2017). Women’s descriptions of childbirth trauma relating to care provider actions and interactions. BMC pregnancy and childbirth, 17(1), 21.
Robohm, J. S., & Buttenheim, M. (1997). The gynecological care experience of adult survivors of childhood sexual abuse: a preliminary investigation. Women & health, 24(3), 59-75.
Roth LM, Heidbreder N, Henley MM, Marek M, Naiman-Sessions M, Torres J and Morton CH. (2014). Maternity Support Survey: A Report on the Cross-National Survey of Doulas, Childbirth Educators and Labor and Delivery Nurses in the United States and Canada.
The epic failure of the evidence-based movement
“All procedures offered to a mother should be researched by herself so she can make an informed decision.”
(posted on Facebook on a thread about routine interventions)“Make sure you hire a doula.”
(said by everyone)
Why are mothers being told to do their own research, find out more about their provider and their hospital, check out the alternatives, and make sure they can make an informed decision?
The pipe on my hot water tank sprung a leak and I called a plumber. Not once was I admonished to check into the possible things he might do to fix it and to decide if it was evidence based or if I should switch plumbers. He did a good job because if he didn’t, it would get around, and no one would hire him again.
And yet, mothers are urged to make sure they find out for themselves the risks of ultrasounds, what the science says about postdates, the risks of synthetic oxytocin (Pitocin/syntocinon), whether an epidural can cause problems, whether Friedman’s curve is actually useful for deciding on a “failure to progress” or if it’s a tool for the hospital to manage their time and resources, whether an induction for a big baby is evidence based, or if their provider supports a VBAC and what the risks are between VBAC and a repeat c-section. And if nothing else, hire a doula. And on it goes.
What’s behind this push for families to do their own research into the routines and interventions of birth? I think it’s been the epic failure of the evidence-based movement.
“All procedures offered to a mother should be researched by herself so she can make an informed decision.”
(posted on Facebook on a thread about routine interventions)
“Make sure you hire a doula.”
(said by everyone)
Why are mothers being told to do their own research, find out more about their provider and their hospital, check out the alternatives, and make sure they can make an informed decision?
The pipe on my hot water tank sprung a leak and I called a plumber. Not once was I admonished to check into the possible things he might do to fix it and to decide if it was evidence based or if I should switch plumbers. He did a good job because if he didn’t, it would get around, and no one would hire him again.
And yet, mothers are urged to make sure they find out for themselves the risks of ultrasounds, what the science says about postdates, the risks of synthetic oxytocin (Pitocin/syntocinon), whether an epidural can cause problems, whether Friedman’s curve is actually useful for deciding on a “failure to progress” or if it’s a tool for the hospital to manage their time and resources, whether an induction for a big baby is evidence based, or if their provider supports a VBAC and what the risks are between VBAC and a repeat c-section. And if nothing else, hire a doula. And on it goes.
What’s behind this push for families to do their own research into the routines and interventions of birth? I think it’s been the epic failure of the evidence-based movement.
Evidence-based medicine
The expression “evidence-based medicine” was introduced in 1991 in an ACP (American College of Physicians) Journal Club editorial and was quickly embraced. Medical clinical practice has been historically referred to as the “art of medicine” where expert opinion, experience and authoritarian judgement were the foundation for decision-making. Medicine held a strong distrust of biomedical research, scientific methodology and statistical analysis (Sur & Dahm, 2011). The problem was that medicine was lagging in accuracy and safety as other disciplines embraced these scientific tools. Obstetrics, in particular, was the medical discipline with the least sound practices, so much so, that Archie Cochrane awarded the discipline of obstetrics with the humiliating “wooden spoon” award in 1979. A decade later, A Guide to Effective Care in Pregnancy and Childbirth was published which seemed to usher in a new approach in obstetrics, and he agreed that it was time to withdraw his insult.
The most widely-accepted definition of evidence-based medicine is as follows:
“Evidence-based medicine [or care] is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research” (Sackett, 1996).
This sounds like the ideal where clients are both treated as individuals and are informed by the most current scientific information. However, this is not the experience of birthing mothers. Instead, mothers throughout the world, where obstetricians are the primary providers and hospitals are the primary birth location, are treated to what is largely a one-size-fits-all approach that resembles Henry Ford’s invention of the assembly line manufacturing plant (Perkins, 2004).
Policies that benefit the institution and the provider have replaced both common sense and holistic care. The widespread ban on VBACs (vaginal births after caesareans) in the US and the near universal unwillingness to support a vaginal breech birth speaks to the profit-before-sense kind of treatment that force women into increasingly unnecessary and risky surgeries without choice or individual care.
It’s also important to consider the limitations of “evidence-based” research. The randomised controlled trial (RCT) has been decided by committee to be the gold standard in research methodology. What this fails to recognise is that a birthing mother is an autonomous human who needs to be given a right to say what happens to her in birth. It’s unethical to randomly assign her to one arm of a research study without her ability to know what her choices are and to make an informed decision. Further, funding drives research. Only certain studies receive funding, which seldom extends beyond a brief time period. When interpreting research, one must consider the question being asked, the conditions under which it was asked, the parameters of the study, potential biases, limitations, and often, false conclusions (Ioannidis, 2005).
Increasing interventions
In the last several years, the rate of obstetrical interventions has increased dramatically without corresponding benefit. Increased interventions in low-risk mothers show an increase in neonatal morbidity (Dahlen et al., 2014). One would think that the evidence-based approach to maternity care would mean a reduced incidence of sick or hurt babies. Instead, money and profit has been a powerful motivator for increased use of interventions. It’s a well-documented fact that a mother in a private facility is more likely to have increased interventions and caesarean surgery than in a public facility. In other words, she’s more likely to have expensive services, like surgery, when she (or her insurance) has more money to offer (Dahlen et al., 2012).
Medical malpractice liability is another factor that influences the high rates of interventions and lessens the choices and autonomy provided to mothers. When the clinician or the facility is worried about being sued, they are more likely to use interventions and perform surgery (Morris, 2015).
Further, there is a direct relationship between a surgeon’s malpractice premiums and the rate of caesarean surgeries. In other words, the more that the provider pays for insurance, the more that caesarean surgeries are performed and the fewer VBACs that are supported (Yang, Mello, Subramanian, & Studdert, 2009).
The rates of interventions vary widely across countries, regions and even hospitals, including caesareans (Kozhimannil, Law, & Virnig, 2013), episiotomies (Graham, Carroli, Davies, & Medves, 2005), inductions (Tenore, 2003), and most every obstetric intervention. Certainly, differences in clientele would influence the rates of interventions in that a mother who is not well would have complications that require medical support. However, even that cannot explain the wide variation in obstetric interventions. The primary predictor of whether a low risk mother will receive a routine intervention is the kind of provider she has (Robinson, Norwitz, Cohen, & Lieberman, 2000).
Outdated practices
ACOG (American Congress of Obstetricians and Gynecologists) themselves admit that only about 25% of their obstetrical practice guidelines are based in good quality research. The rest is based in poor quality studies, opinion, and habit (Wright et al., 2011). The SOGC’s (Society of Obstetricians and Gynaecologists of Canada) practice guidelines are not much different in content. And frankly, no matter what the evidence says, most mothers get what’s offered and that’s often outdated protocols based on poor quality information, or habit.
We’ve known for 30 years that routine episiotomy, cutting the perineum to make a larger passage for the baby at birth, causes increased 3rd and 4th degree lacerations, increased fecal incontinence, and increased pain that can last years (Thorpe, Bowes Jr, Brame, & Cefalo, 1987; Borgatta, Piening, & Cohen, 1989; Klein et al., 1992; Signorello, Harlow, Chekos, & Repke, 2000; Hartmann et al., 2005). While the rate of episiotomies has been falling in most locations, according to the Listening to Mothers III Survey (US), 17% of women still had this procedure (Declercq, Sakala, Corry, Applebaum, & Herrlich, 2013).
“During the 40 minutes of pushing, the doctor turned to my mother and said, “I’m cutting her” and I yelled and begged for her NOT to cut me. But she ignored me and did it anyways. When she started to stitch me up, once again, I was screaming and begging for her to stop because it was extremely painful. I didn’t even know they were supposed to numb you first until recently.” (Carol, personal communication, 2016)
Back in the 1940’s it became routine to deny a mother any food in labor since she was going to be put under general anesthesia for her birth. The concern was that she would vomit under anesthesia and then aspirate (breathe) in the vomit and possibly die from the complications. Interestingly, it’s also been know for almost 30 years that fasting during labour doesn’t ensure gastric emptying (an empty stomach) and instead increases the acidity in her stomach, which is more problematic. And in fact, the likelihood of a mother dying from aspirating vomit during an emergency caesarean under general anesthesia is about 7 in 10,000,000 births (Sleutel & Golden, 1999). Further, forced fasting leads to a longer pushing stage (Rehamani, Khakbazan, Yavari, Granmayeh, & Yavari, 2012). No doubt that’s because labour burns up to 1000 calories per hour and the mother just gets tired from lack of nourishment.
The original recommendation in the 1940’s was based on worry and an attempt to exercise caution. There has been no corroborating evidence since then and any research has shown that eating and drinking brings comfort to mothers and reduces both pain and length of labour, so there is no reason to restrict the food they want (Singata, Tranmer, & Gyte, 2010). And yet, most mothers are not “allowed” to eat during labour when they birth in a hospital due to outdated and inflexible policies. Adding in a routine IV with glucose to replace real food just increases problems, as those newborns are more likely to have serious low blood sugar (Grylack, Chu, & Scanlon, 1984). So why aren’t most mothers eating in labour? Because hospitals don’t change outdated practices when it’s still working for them. Not providing food for labouring mothers saves money.
There are so many non-evidence based routines happening every day including:
Caesareans for failure to progress based on outdated time limits (Laughon, Branch, Beaver, & Zhang, 2012)
Routine induction at early term with a membrane stripping (Hill et al., 2008)
Routine induction for suspected fetal macrosomia (big baby) (Boulvain, Irion, Dowswell, & Thornton, 2016)
Induction for isolated (no other medical complications) oligohydramnios (low amniotic fluid) at term (close to your due date) (Manzanares et al., 2007)
Induction for isolated (no other complications) hypertension (high blood pressure) near term (Broekhuijsen et al., 2015)
Birthing on your back with your feet in the air or in stirrups, called a supine delivery (Terry, Westcott, O'Shea, & Kelly, 2006)
Staying in bed for labour (Bloom et al., 2008)
Continuous electronic fetal monitoring (Alfirevic, Devane, & Gyte, 2013)
Mandatory surgery for a breech presentation (Louwen, Daviss, Johnson, & Reitter, 2016)
Immediate cord clamping (Hutton, Reitsma, & Kaufman, 2007)
And on it goes.
“I remember telling my first doctor that I didn’t want or need rhogam at 27 weeks. I had researched it and because both my husband and I were negative blood type, it was impossible to have a positive baby. She told me I had no choice. It was mandatory.” (Joanne, personal communication, 2016)
How bad is it?
Consider that in the survey, Listening to Mothers III (US) (Declercq et al., 2013)
80% did not eat during labour
68% of mothers birthed on their backs
55% did not walk or move around during active labour
44% were induced for the reason that they were merely at term
16% were induced because the doctor was worried about a large baby
11% were induced because the doctor was worried about low fluid at term
10% had their public hair shaved for a vaginal birth
and when making a decision to have a repeat c-section rather than attempt a VBAC 63% said it was the doctor who made the decision
According to BORN Ontario (Niday Perinatal Database) 2005-2006 to 2009-2010 (BORN, 2011)
Inductions have risen from 21.8% in 2005-6 to 25.2% in 2009-10. A 15.6% increase in just 4 years cannot be explained by a massive shift in maternal-fetal wellbeing, but rather speaks to how quickly practitioners choose an intervention on a broad scale.
The rate of repeat c-sections increased 28.6% over that same time period
57.6% of elective repeat caesareans were performed before 39 weeks
18.3% of mothers had an episiotomy.
The caesarean section rate has increased every year across Canada from 18.7% in 1997 to 27.5% in 2014 where repeat surgery makes up more than half of this rise (CIHI, 2016). It seems that scheduled, profitable, daylight obstetrics is the driver behind this as there has been no new evidence of increased risk or harm to mothers or babies from VBAC births in the last several years.
What is stunning is that in spite of the evidence based movement, maternal mortality has risen in the US between 1990 and 2013 from 12 deaths per 100,000 to 28 per 100,000. Lack of consistent obstetrical practices has been identified as a major concern in this rising rate (Agrawal, 2015). And given the high rates of caesarean surgery, often due to policy or insurance premiums, it’s necessary to count the cost in lives lost due to excessive rates of surgery. Postpartum death is 3.6 times higher after a surgical birth than a vaginal birth (Deneux-Tharaux, Carmona, Bouvier-Colle, & Bréart, 2006).
In Canada, maternal mortality increased from 6 per 100,000 in 1990 to 11 per 100,000 in 2013. The question that begs to be answered is, where does the shocking increase in surgical birth fit into this decline in maternal safety?
Obstetric violence
In 2007, Venezuela became the first country to define obstetric violence through the Organic Law on the Right of Women to a Life Free of Violence.
In this law, obstetric violence is defined as:
“The appropriation of the body and reproductive processes of women by health personnel, which is expressed as dehumanized treatment, an abuse of medication, and to convert the natural processes into pathological ones, bringing with it loss of autonomy and the ability to decide freely about their bodies and sexuality, negatively impacting the quality of life of women.”
The following acts, executed by care providers, are considered obstetric violence:
1. Untimely and ineffective attention of obstetric emergencies;
2. Forcing the woman to give birth in a supine position, with legs raised, when the necessary means to perform a vertical delivery are available;
3. Impeding the early attachment of the child with his/her mother without a medical cause thus preventing the early attachment and blocking the possibility of holding, nursing or breast-feeding immediately after birth;
4. Altering the natural process of low-risk delivery by using acceleration techniques, without obtaining voluntary, expressed and informed consent of the woman;
5. Performing delivery via cesarean section, when natural childbirth is possible, without obtaining voluntary, expressed, and informed consent from the woman.
Obstetric violence is global and systemic (WHO, 2014). Having procedures performed that introduce risk without their knowledge or consent routinely violates mothers. Having her membranes broken in a healthy labour without indication, or having synthetic oxytocin unknowingly introduced into their IV, being forced onto her back for delivery, or having her genitals cut against her wishes are just the tip of the iceberg.
And yet, no one is holding the industry accountable. Obstetrical societies (ACOG, SOGC, et. al.) maintain a powerful lobbying presence with government to ensure that public policies and government spending are favourable to their industry. An absence of adequate oversight has allowed this industry to escalate their intrusion into healthy pregnancies to the point where 1 in 3 mothers say their births were traumatic and up to 1 in 10 mothers are grappling with postpartum PTSD as a result of their birthing experience (Beck, Gable, Sakala, & Declercq, 2011).
“I had a successful VBAC in a hospital. The next thing I know, an entire arm, up to her elbow, shoots into my vagina and uterus without any warning. I felt every inch of my placenta being ripped out of my uterus. I screamed at her to stop. Instead, the nurse pinned me down. PTSD robbed me of the next year of my life.” (Marie, personal communication, 2016)
The fact that the industry will not hold those providers and those institutions accountable for dangerous, outdated, and at times, abusive practices is simply stunning. Lateral violence (bullying, insults, coercion, sabotage, and even physical assault) within the industry keeps whistle blowers from speaking up, in particular nurses (Jackson et al., 2010). Nurses are especially vulnerable to lateral violence as the vast majority of nurses have been victims, most often from senior nurses (Christie, Jones, & PMHNPBC, 2014). This impacts their delivery of care to their patients and patient safety. In hospitals, nurses are the primary contact with the birthing family and the one in the best position to advocate for her patient and to report abusive or outdated care. Abusive behaviour within the nursing profession has contributed to preventing them from appropriately dealing with this failure on the part of the industry to give mothers the care they need and deserve.
The birth monopoly
Through clever marketing and expensive lobbying, obstetrics has gained a monopoly on birth. In most developed nations, hospitals have cornered the market on birth services and obstetricians, although more expensive and associated with more adverse outcomes in low risk populations, are the primary provider for most women. In places where midwifery is integrated into the health system, meaning they can facilitate a transfer to a hospital where her client will be accepted and the transfer is respectful and seamless, mothers have better outcomes at home with a midwife (Hutton, Reitsma, & Kaufman, 2009).
Physicians themselves are punished for providing true family centred care and risk losing hospital privileges for supporting a homebirth where the money doesn’t reach the institution. Like a dangerous cult, adherents (obstetricians) have even pursued a court order to force a mother to undergo mandatory caesarean surgery or called in child protective services to apprehend the children of mothers who disobeyed their dictates (Diaz-Tello, 2016).
“After 2 attempted homebirths that ended in caesareans, I was told that no midwife or doctor would support plans to have a homebirth VBAC. I could attempt a hospital VBAC but I would have to “fight” for it. To plan to attempt a vaginal birth at the same hospital, knowing that I would have to resist the system and medical staff every step of the way, was a recipe for failure and emotional distress.” (Lainie, personal communication 2016)
A few good folks
This is an industry-wide problem. However, there are truly wonderful individual providers who are doing their best to provide sensitive and individualised care with the best information they have. And they deserve credit, respect and thanks. Both doctors and midwives are routinely refused the opportunity to serve their clients in the manner they wish, perhaps through offering vaginal breech support, or not inducing according to policy when there is no medical indication. Yet these brave providers offer this care in the face of potentially sabotaging their opportunities for career advancement.
These providers are in high demand and are sometimes vilified by their colleagues whose excessive interventions bring more money into the industry coffers. They are shining diamonds in a deep mine and they make a difference in the lives of those fortunate enough to find them.
Individual nurses have taken the brunt of institutional hostility for advocating for their clients, for reporting unsafe practices, and for holding their colleagues to a higher standard. These are the professionals who deserve support and accolades.
Indeed, the evidence-based movement has been an epic failure that has left families reeling from their inability to influence their providers or the system that has set itself up to “save” her and her baby.
Families are paying the price
The true failure of the evidence-based movement has been the toll exacted on birthing families through lack of autonomy, lack of choice, excessive interventions, excessive surgery, birth trauma, and lives lost.
Due to the failure of the industry to deliver on their promise, we’ve entered the age where evidence based-medicine has become the responsibility of the consumer. Birthing families are urged to learn what their provider won’t learn or won’t practice.
When they are caught in a system run by dinosaurs, they are told that they didn’t do their research, they didn’t hire a doula, or they didn’t advocate for themselves. And the industry eats this up. They tell mothers to come in with a birth plan, all the while knowing that they see a birth plan as a direct route to more interventions (Grant, Sueda, & Kaneshiro, 2009).
A switch to a midwifery model of care with midwives providing the bulk of maternity services would mitigate some of these issues, as they’re more likely to use evidence-based care and to engage in informed consent and mother-centred care (Sandall, Soltani, Gates, Shennan, & Devane, 2016). However, a profitable industry with well-paid lobbyists won’t give up power and control easily. Obstetrics is currently a one-stop shop that provides a drive-through experience where everyone gets what’s on the menu.
You’ll note that when drawing attention to the need for mothers to do their own research or cautioning them to learn more about their provider before they consent to a routine, we hear total nonsense from industry members about not scaring mothers, not spreading misinformation, going with the flow, staying off the internet, and trusting the professionals. What they should be doing is apologising for aiding and abetting outdated protocols and industry-favourable policies that hurt mothers and babies and that it’s time to hold themselves accountable and rise to a higher standard.
Indeed, the evidence-based movement has been an epic failure that has left families reeling from their inability to influence their providers or the system that has set itself up to “save” her and her baby.
"I left the care of midwives when I caught them in lies and practices that went against informed choice. Despite what the medical system would have you believe, I had a wonderful and safe VBAC at home without a medical professional." (Chahna, personal communication, 2016)
The grassroots move to a new paradigm
Humans are resilient and they’ve always found a way to step away from systems that feel oppressive and to form communities that chart a path that honours their values, despite the risk of persecution. The rise of the DIY (do it yourself) birth movement, also called freebirth, unassisted, or family birth is a grassroots response that sees families taking care of each other outside of the obstetrical industry. There’s been a rise in unassisted homebirths in Sweden, Australia, Canada, the US, and Finland in response to the biomedical approach to birth and lack of autonomy for birthing mothers (Holten & de Miranda, 2016).
Of course, the obstetrical industry sees this as an exceptionally dangerous movement. Yet, their warnings may not match up with the experiences of the families themselves and may be more related to their position as a monopoly than the evidence of the safety of birth outside of their oversight.
In an anonymous online survey from December 2014 until September 2015, mothers who planned an unassisted birth responded (O’Day, 2016).
857 respondents from around the world
1449 babies born
1444 births (5 sets of twins)
1339 babies were born “unassisted”, meaning that there was no licensed attendant present although there might have been family, friends, doulas, or unregistered midwives.
The primary reason for choosing an unassisted birth was that they were led by their intuition (80.24%). The next most common reason was their dislike of hospitals (77.32%). They were also concerned for their newborn’s safety within a hospital setting (72.2%) and did not want to repeat a prior bad hospital experience (51.83%).
The results were interesting in the extraordinarily positive outcomes.
There were no maternal deaths
The neonatal death rate was 2.2 per 1000, which is comparable to the US rate of 2.97 per 1000
The caesarean rate was 1.24%
Of those who attempted a VBAC, 100% achieved it
Of those who had a VBAC, just over one quarter had had more than one previous caesarean
One third of the mothers had no prenatal services with a licensed provider, also called ‘prenatal care’ (this doesn’t account for community care and wellness measures)
Over 70% had no monitoring throughout labour and birth, i.e. no one listening to the baby’s heartbeat or routine vaginal exams
Just over 2% transported the newborn to a medical facility within the first week, mostly for breathing concerns
3.52% of the mothers transported for medical help after the baby was born primarily for postpartum haemorrhage
Certainly, this is a self-selecting group who responded to this survey. However, given that some of them were “high risk” in that they had had previous caesareans, had no prenatal care, and 5 were expecting twins, these results are seldom found within the medical obstetrical industry.
Once I decided not to continue prenatal care with the registered midwives, I was easily able to avoid trauma triggers and enjoy my pregnancy a lot more. The birth of my third baby was awesome! I was free to move around the whole house, I could eat or drink when I felt like it, I didn't have a single exam and I slept when I felt tired. I wasn't alone, but the people who were there didn't disturb me in any way. I never once wanted drugs for pain or to go to the hospital, it wasn't an option for me. My daughter had the best birth. No trauma, drama, drugs, strangers or tearing. Just a simple, healthy, happy family birth. (Samantha, personal communication, 2016)
© Billie Harrigan Consulting
As consumers have come to understand that the onus for evidence-based medicine has fallen on their shoulders, they’ve responded with outreach and connection. Online groups connect families to each other where they share research, studies, tips and encouragement. They share their medical history with one another and offer suggestions for self-care as well as recommendations for those providers and traditional birth attendants who support clients with holistic and scientifically sound care.
In-person groups are gathering to teach one another the physiology of birth, the mechanics of a vaginal breech birth, how to resolve a shoulder dystocia or a head entrapment, and to practice neonatal resuscitation skills.
Doulas are investing in advanced education and research skills to support their clients’ wishes for the evidence, access to their provider’s practice guidelines, and community connections and alternative care. Doulas are becoming specialists in supporting self-advocacy, research-based information, and helping clients connect to the services they need and want.
And as we learn more, we’re also discovering the importance of our microbiome and the epigenetic expression of our DNA where today’s one-size-fits-all comes across as pure buffoonery.
Taking back birth
We are at a crossroads in human history that will unfold over time. The “take back birth” movement is gaining momentum and this is being met with religious like zeal from the industry and its adherents in its opposition. They preach a different gospel where the modern medicalisation of birth and wholesale institutionalisation of birthing women has “saved” them. It’s a gospel that doesn’t hold up to scrutiny but nonetheless forms the lexicon of our culture (Tew, 2013).
So what can families do in light of the epic failure of evidence-based medicine?
Perhaps the answer lays in common sense.
Common sense dictates that if frequent prenatal visits and testing is upsetting, that the individual could just choose to bypass many of them. Science affirms that prenatal testing, no matter the results, increases maternal anxiety (Allison, Stafford, & Anumba, 2011). Prenatal anxiety is a risk factor for postpartum PTSD after a traumatic birth (Söderquist, Wijma, Thorbert, & Wijma, 2009). Maternal anxiety is also associated with poorer birth outcomes (Kumari & Joshi, 2014). And skipping those visits actually has no adverse outcome on the mum and baby and only affects the provider’s pocketbook (Walker, McCully, & Vest, 2001).
Common sense tells us that if a technology is useful for breaking up tissues such as cysts, scar tissue or kidney stones because it moves cells, then it might not be entirely safe for developing fetuses. Many parents are wary of ultrasound and their instincts tell them to bypass this routine. In fact, routine and frequent ultrasounds can contribute many problematic issues and has still not shown any benefit to mothers and babies, however it does increase inductions and caesareans (Cohain, 2011).
Common sense tells us that if we don’t want the gloved hand of someone we’re not in an intimate relationship with in our vaginas, we might want to decline as it may be more problematic than helpful (Lenihan, 1984).
Common sense suggests that if a hospital isn’t your cup of tea then birthing at home is a reasonable option (NICE, 2014).
Common sense and science are often aligned beautifully and generally support an individualistic approach to wellness, including birth, which takes into account a birthing mother’s physical, social, spiritual, and relational complexities. And as we learn more, we’re also discovering the importance of our microbiome and the epigenetic expression of our DNA where today’s one-size-fits-all comes across as pure buffoonery.
It’s going to be interesting to see how the medical industry responds to this growing grassroots movement. No doubt, lobbyists will pursue legislation to force mothers into the system for profit under the guise of “safety” which will drive families deeper underground. And should the numbers of families who choose to give birth outside the system actually have an impact on the profit margin of hospitals and obstetrical practices, then we’ll see a swift shift to “evidence-based” and “family-centred” care.
Until then, those good providers will do the best they can. Doulas will equip their clients with science and resources. And families will connect to support one another on this journey.
Evidence-based care has been an epic failure for parents but a mighty gold strike for the industry as they’ve cashed in on an illusion.
“I wish I knew then that I had the power to say NO. This is my body and we’re going to do this my way.” (Janice, personal communication, 2016)
References
Agrawal, P. (2015). Maternal mortality and morbidity in the United States of America. Bulletin of the World Health Organization, 93(3), 135-135.
Alfirevic, Z., Devane, D., & Gyte, G. M. (2013). Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. The Cochrane Library.
Allison, S. J., Stafford, J., & Anumba, D. O. (2011). The effect of stress and anxiety associated with maternal prenatal diagnosis on feto-maternal attachment. BMC women's health, 11(1), 1.
Beck, C. T., Gable, R. K., Sakala, C., & Declercq, E. R. (2011). Posttraumatic stress disorder in new mothers: Results from a two‐stage US National Survey. Birth, 38(3), 216-227.
Better Outcomes Registry & Network (BORN) Ontario. (2011). Perinatal Health Report 2009-2010. Greater Toronto Area (GTA) - LIHNs 5 to 9. Ottawa ON.
Bloom, S. L., McIntire, D. D., Kelly, M. A., Beimer, H. L., Burpo, R. H., Garcia, M. A., & Leveno, K. J. (1998). Lack of effect of walking on labor and delivery. New England Journal of Medicine, 339(2), 76-79.
Borgatta, L., Piening, S. L., & Cohen, W. R. (1989). Association of episiotomy and delivery position with deepperineal laceration during spontaneous delivery in nulliparous women. American journal of obstetrics and gynecology, 160(2), 294-297.
Boulvain, M., Irion, O., Dowswell, T., & Thornton, J. G. (2016). Induction of labour at or near term for suspected fetal macrosomia. The Cochrane Library.
Broekhuijsen, K., van Baaren, G. J., van Pampus, M. G., Ganzevoort, W., Sikkema, J. M., Woiski, M. D., ... & Rijnders, R. J. (2015). Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): an open-label, randomised controlled trial. The Lancet, 385(9986), 2492-2501.
Canadian Institute for Health Information, & Canadian Population Health Initiative. (2016). Improving the Health of Canadians. Summary Report [electronic Resource]. Canadian Institute for Health Information.
Christie, W., Jones, S., & PMHNPBC, R. (2014). Lateral violence in nursing and the theory of the nurse as wounded healer. OJIN: The Online Journal of Issues in Nursing, 19(1).
Cohain, J. S. (2011). Prenatal ultrasound does not improve perinatal outcomes. Midwifery today with international midwife, (102), 46-7.
Dahlen, H. G., Tracy, S., Tracy, M., Bisits, A., Brown, C., & Thornton, C. (2012). Rates of obstetric intervention among low-risk women giving birth in private and public hospitals in NSW: a population-based descriptive study. BMJ open, 2(5), e001723.
Dahlen, H. G., Tracy, S., Tracy, M., Bisits, A., Brown, C., & Thornton, C. (2014). Rates of obstetric intervention and associated perinatal mortality and morbidity among low-risk women giving birth in private and public hospitals in NSW (2000–2008): a linked data population-based cohort study. BMJ open, 4(5), e004551.
Declercq, E. R., Sakala, C., Corry, M. P., Applebaum, S., & Herrlich, A. (2013). Listening to MothersSM III.
Deneux-Tharaux, C., Carmona, E., Bouvier-Colle, M. H., & Bréart, G. (2006). Postpartum maternal mortality and caesarean delivery. Obstetrics & Gynecology, 108(3, Part 1), 541-548.
Diaz-Tello, F. (2016). Invisible wounds: obstetric violence in the United States. Reproductive Health Matters.
Graham, I. D., Carroli, G., Davies, C., & Medves, J. M. (2005). Episiotomy rates around the world: an update. Birth, 32(3), 219-223.
Grant, R., Sueda, A., & Kaneshiro, B. (2009). Expert opinion vs. patient perception of obstetrical outcomes in laboring women with birth plans. The Journal of reproductive medicine, 55(1-2), 31-35.
Grylack, L. J., Chu, S. S., & Scanlon, J. W. (1984). Use of intravenous fluids before caesarean section: effects on perinatal glucose, insulin, and sodium homeostasis. Obstetrics & Gynecology, 63(5), 654-658.
Hartmann, K., Viswanathan, M., Palmieri, R., Gartlehner, G., Thorp, J., & Lohr, K. N. (2005). Outcomes of routine episiotomy: a systematic review. Jama, 293(17), 2141-2148.
Hill, M. J., McWilliams, G. D., Garcia-Sur, D., Chen, B., Munroe, M., & Hoeldtke, N. J. (2008). The effect of membrane sweeping on prelabor rupture of membranes: a randomized controlled trial. Obstetrics & Gynecology, 111(6), 1313-1319.
Holten, L., & de Miranda, E. (2016). Women׳ s motivations for having unassisted childbirth or high-risk homebirth: An exploration of the literature on ‘birthing outside the system’. Midwifery.
Hutton, E. K., & Hassan, E. S. (2007). Late vs early clamping of the umbilical cord in full-term neonates: systematic review and meta-analysis of controlled trials. Jama, 297(11), 1241-1252.
Hutton, E. K., Reitsma, A. H., & Kaufman, K. (2009). Outcomes Associated with Planned Home and Planned Hospital Births in Low‐Risk Women Attended by Midwives in Ontario, Canada, 2003–2006: A Retrospective Cohort Study. Birth, 36(3), 180-189.
Ioannidis, J. P. (2005). Why most published research findings are false. PLoS Med, 2(8), e124.
Jackson, D., Peters, K., Andrew, S., Edenborough, M., Halcomb, E., Luck, L., ... & Wilkes, L. (2010). Trial and retribution: A qualitative study of whistleblowing and workplace relationships in nursing. Contemporary nurse, 36(1-2), 34-44.
Klein, M. C., Gauthier, R. J., Jorgensen, S. H., Robbins, J. M., Kaczorowski, J., Johnson, B., ... & Gelfand, M. M. (1992). Does episiotomy prevent perineal trauma and pelvic floor relaxation?. The Online journal of current clinical trials, 6019-words.
Kozhimannil, K. B., Law, M. R., & Virnig, B. A. (2013). Caesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Affairs, 32(3), 527-535.
Kumari, S., & Joshi, S. (2014). Birth outcomes following antenatal anxiety and depression.
Laughon, S. K., Branch, D. W., Beaver, J., & Zhang, J. (2012). Changes in labor patterns over 50 years. American journal of obstetrics and gynecology, 206(5), 419-e1.
Lenihan Jr, J. P. (1984). Relationship of antepartum pelvic examinations to premature rupture of the membranes. Obstetrics & Gynecology, 63(1), 33-37.
Lothian, J. (2006). Birth plans: the good, the bad, and the future. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 35(2), 295-303.
Louwen, F., Daviss, B. A., Johnson, K. C., & Reitter, A. (2016). Does breech delivery in an upright position instead of on the back improve outcomes and avoid caesareans?. International Journal of Gynecology & Obstetrics.
Manzanares, S., Carrillo, M. P., Gonzalez-Peran, E., Puertas, A., Montoya, F., Manzanares, S., ... & Montoya, F. (2007). Isolated oligohydramnios in term pregnancy as an indication for induction of labor. The Journal of Maternal-Fetal & Neonatal Medicine, 20(3), 221-224.
Morris, T. (2013). Cut it out: the C-section epidemic in America. NYU Press.
National Institute for Health and Care Excellence (NICE). (2014) Intrapartum care for healthy women and babies. Clinical guideline CG190.
O’Day, Katharine L. (2016). “Outside the System”: Motivations and Outcomes of Unassisted Childbirth. Published Online November 19, 2016, Sacred Transitions Midwifery Institute.
Perkins, B. B. (2004). The medical delivery business: Health reform, childbirth, and the economic order. Rutgers University Press.
Rahmani, R., Khakbazan, Z., Yavari, P., Granmayeh, M., & Yavari, L. (2012). Effect of oral carbohydrate intake on labor progress: randomized controlled trial. Iranian journal of public health, 41(11), 59.
Robinson, J. N., Norwitz, E. R., Cohen, A. P., & Lieberman, E. (2000). Predictors of episiotomy use at first spontaneous vaginal delivery. Obstetrics & gynecology, 96(2), 214-218.
Sackett, D. L. (1997, February). Evidence-based medicine. In Seminars in perinatology (Vol. 21, No. 1, pp. 3-5). WB Saunders.
Sandall, J., Soltani, H., Gates, S., Shennan, A., & Devane, D. (2016). Midwife‐led continuity models versus other models of care for childbearing women. Cochrane database of systematic reviews, (4).
Signorello, L. B., Harlow, B. L., Chekos, A. K., & Repke, J. T. (2000). Midline episiotomy and anal incontinence: retrospective cohort study. Bmj, 320(7227), 86-90.
Singata, M., Tranmer, J., & Gyte, G. M. (2010). Restricting oral fluid and food intake during labour. The Cochrane Library.
Sleutel, M., & Golden, S. S. (1999). Fasting in labor: relic or requirement. Journal of Obstetric, Gynecologic & Neonatal Nursing, 28(5), 507-512.
Söderquist, J., Wijma, B., Thorbert, G., & Wijma, K. (2009). Risk factors in pregnancy for post‐traumatic stress and depression after childbirth. BJOG: An International Journal of Obstetrics & Gynaecology, 116(5), 672-680.
Sur, R. L., & Dahm, P. (2011). History of evidence-based medicine. Indian Journal of Urology, 27(4), 487.
Tenore, J. L. (2003). Methods for cervical ripening and induction of labor. American family physician, 67(10), 2123-2128.
Terry, R. R., Westcott, J., O'Shea, L., & Kelly, F. (2006). Postpartum outcomes in supine delivery by physicians vs nonsupine delivery by midwives. The Journal of the American Osteopathic Association, 106(4), 199-202.
Tew, M. (2013). Safer childbirth?: a critical history of maternity care. Springer.
Thorp Jr, J. M., Bowes Jr, W. A., Brame, R. G., & Cefalo, R. (1987). Selected use of midline episiotomy: effect on perineal trauma. Obstetrics & Gynecology, 70(2), 260-262.
Walker, D. S., McCully, L., & Vest, V. (2001). Evidence‐based prenatal care visits: When less is more. Journal of Midwifery & Women’s Health, 46(3), 146-151.
World Health Organisation. (2014). The prevention and elimination of disrespect and abuse during facility-based childbirth: WHO statement.
Wright, J. D., Pawar, N., Gonzalez, J. S., Lewin, S. N., Burke, W. M., Simpson, L. L., ... & Herzog, T. J. (2011). Scientific evidence underlying the American College of Obstetricians and Gynecologists' practice bulletins. Obstetrics & Gynecology, 118(3), 505-512.
Yang, Y. T., Mello, M. M., Subramanian, S. V., & Studdert, D. M. (2009). Relationship between malpractice litigation pressure and rates of caesarean section and vaginal birth after caesarean section. Medical care, 47(2), 234.