Why I don't do vaginal exams ~ Wisdom from a Traditional Birth Companion
I let my new client know what would happen when I arrived at her home when she was in labour. We talked about sanitation measures, spending time in the kitchen, setting up the pool, and where I could take a nap if she needed some privacy. I said I would not be doing any vaginal exams as I think they’re rude, and she wept with relief.
I specialise in trauma and the majority of my clients are refugees from the medical system, running from ritual abuse and routines that protect the industry. They want someone to mentor them through to a healthy birth without the traps and trappings of the industry that removed their choice, and violated their autonomy and their dignity.
As a traditional birth attendant, I don’t do vaginal exams.
I was talking with my new client about what would likely happen when I arrived at her home when she was in labour. We talked about sanitation measures, spending time in the kitchen, setting up the pool, and where I could take a nap if she needed some privacy. I said I would not be doing any vaginal exams as I think they’re rude, and she wept with relief.
I specialise in trauma and the majority of my clients are refugees from the medical system, running from ritual abuse and routines that protect the industry. They want someone to mentor them through to a healthy birth without the traps and trappings of the industry that removed their choice, and violated their autonomy and their dignity.
We won’t go into the history of obstetrics that began with the burning of witches (midwives and healers), the rise of the man-midwife, the development of lying-in hospitals, and eventually the wholesale co-opting and medicalisation of birth. Suffice it to say that obstetrics and hospitalisation didn’t “save” women and babies (1). It created untold harm and mortality until they learned better infection control and saner behaviours. Today, it’s still leaving a trail of destruction as about 1/3 of their clients are traumatised (2,3,4) and about 1 in 8 enter parenthood with postpartum post-traumatic stress disorder (5,6,7). Suicide is a leading cause of maternal death in the first year and is highly correlated to trauma (8,9,10,11,12,13,14,15,16). It’s an industry out of control with unjustifiable caesarean rates, dangerous inductions for spurious reasons, and wholesale overuse of medications and interventions.
What women didn’t notice in this process of medicalisation and co-opting of their physiology for profit is that the medical industry took ownership of their vaginas once they became pregnant. Pregnancy transfers ownership of the vagina from the woman to the industry. Midwifery and obstetrical regulations stipulate that inserting an instrument, hand, or finger beyond the labia majora is a restricted practice sanctioned by legislation (17). To test this, see how long it takes for someone in the industry to file a Cease and Desist or start a campaign of persecution for the purpose of prosecution if they catch wind of anyone but one of their own sticking their fingers up there. No one but an insider sticks their fingers into their territory. It doesn’t matter who the mother gives her permission and consent to - it must be a member of the priesthood of modern medicine.
Of course, in their benevolence, they’re generally quite accommodating where partners are concerned, because most partners are male and obstetrics is exceedingly misogynistic. They value the needs and the pleasures of the D.
As a traditional birth attendant, I don’t do vaginal exams. For one thing, it’s considered a restricted practice for just the medical pundits and not doing them with my clients keeps the industry players somewhat placated knowing I’m not intruding into their turf. But the real reason is because I think they’re completely unnecessary and wouldn’t do them even if the medical folks begged me to under the guise that it would make birth safer.
To better understand the offence of the routine vaginal exam, we have to go back in time to when the male-midwife moved into the sanctity of women-centred birth and the domain of the midwife. It was profitable. And they convinced the public that they would provide a superior service based on the cultural belief of the time that women were disadvantaged by an inferior intellect and a predilection for sorcery (18,19). They also brought with them the medical perspective that women were an error of nature and that the world, and thus its inhabitants, were but a machine that could be best understood by coming to know its parts in isolation of the whole.
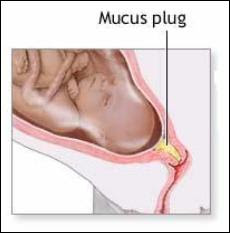
And so began dissection, mechanisation, and reducing birthing women to their parts. She became a womb expelling a foetus through a vagina. Think of today’s obstetrical “power, passenger, passage” perspective on how birth unfolds. Not much has changed in 400 years.
By sticking their fingers up there, they discovered that the cervix opens to expel the foetus. Oh, happy day! From the morgue to the birth suite, physician fingers were poking everything. Throughout the early and mid 1800’s, the infection rate in some hospitals soared as high as 60% from the mysterious childbed fever, with death rates as high as 1 in 4 (20). Nothing the doctors did was contributing to this mystery as physicians were gentlemen and gentlemen didn’t carry germs (21). And once they did accept that their filthy practices were killing women, rather than abandon the idiocy of penetrating their patients in labour, they eventually figured out how to make it less dangerous.
The practice of obstetrics has always been highly resistant to change and common sense. After all, they’ve had 400 years to figure things out and women are still birthing on their backs!
Once it was discovered that the cervix dilates as part of the labouring process, the medical industry has been fixated on that bit of tissue and made it the focus of their entire assembly line drive-through everyone-gets-what’s-on-the-menu service. That bit of tissue determines how the ward allocates services, whether the client will be permitted to stay, and how long she’ll be allowed to use their services before the next client needs the bed.
Thanks to Dr. Emanuel Friedman, who examined the cervices of 500 sedated first-time mothers in the 1950’s and plotted their dilation on a graph and matched it to the time of their birth – we now have the infamous Friedman’s Curve and the partogram.
© Evidence Based Birth
The partogram is a graph that plots cervical dilation and descent of the foetal head against a time-line. When the graph indicates that progress is slower than is allowable according to the particular chart chosen by their institution, then the practitioner is called upon to administer various interventions to speed things up to keep the labour progressing well, aka, profitably. Should these acceleration measures fail to produce a baby in a timely manner or cause foetal distress, then a caesarean section is the solution. “Failure to progress”, and the accompanying foetal distress that is often a consequence of those acceleration measures, are the leading causes of a primary caesarean (22).
Obstetrical partogram
In addition to clearing the bed for the next client, obstetrics has another reason for expediting labour. The more vaginal exams a woman receives, the greater the likelihood she’ll develop a uterine infection (23). So, once they start the poking, they need to get the baby out before their prodding adds another problem for them to solve.
In the absence of a medical situation, routine vaginal exams in labour are for the purpose of charting in order to maintain a medicalised standard of modern technocratic birth.
A labouring client will not be admitted to a hospital without a vaginal exam to determine if her dilation is far enough along for their services (unless she’s clearly pushing). And this isn’t necessarily a bad thing. Early admission to the hospital results in more interventions and more caesareans than later admission (24). This is a business and time is money.
A regulated midwife attending a homebirth will likewise perform a vaginal exam upon arrival at the client’s home to determine if the client is far enough along to warrant their limited resources and time by staying and beginning the partogram or leaving and waiting to be called back later. They must also follow the rules of the hospital at which they have privileges or their regulatory agency and transport for augmentation/acceleration if the partogram shows a significant variation.
All of this is predicated on the outdated and obsolete notion that women are machines and birth is a linear process. The only thing a vaginal exam reveals is where the cervix is sitting at that particular moment and how it’s interpreted by that particular practitioner. Women are not machines and birth is not linear. Just like any mammal, birth can be slowed, stopped, or sabotaged by an unfavourable environment or reckless attendants. I’ve said for years that it’s so easy to sabotage a good birth, it’s embarrassing.
“Years ago, I was with a first-time mother planning a family-centred homebirth. She was on the clock and had a deadline. At 42 weeks gestation, she had until midnight that night to produce a baby in order to have a midwife-attended homebirth. After that, she was expected to report to the hospital for a chemical induction. As her contractions built throughout the day, her preferred midwife arrived and labour was progressing well. She was enjoying the process and the camaraderie of her sisters-in-birth. Eventually, one of the vaginal exams revealed a cervical dilation of 8 cm, indicating it was time to call in the 2nd midwife. Only, it was a midwife that had routinely upset the mother throughout pregnancy with requests for various tests and talk of all the dangers of declining routine testing. Upon learning this midwife was coming to the birth, labour slowed.
Soon enough, the 2nd midwife arrived and assumed authority over the birth process and insisted on repeated vaginal exams for the purpose of staying within the parameters of the partogram. Her vaginal exams were excruciating, no doubt because she was trying to administer a non-consenting membrane stripping as an intervention to address the slowed and almost non-existent contractions. Eventually, an exam revealed a dilation of only 6 cm. After several more hours of “torture” (according to this mother’s recount) to keep labour going rather than just leaving the mother to rest and accepting that this labour had been hijacked and needed time to regroup and restart, dilation regressed to 4 cm and the mother eventually ended up acquiescing to a hospital transfer, and experienced an all-the-bells-and-whistles birth, trauma, and postpartum PTSD.
This mother’s subsequent birth a couple of years later didn’t include inviting midwives and unfolded as it was meant to. After a day of productive and progressing labour that was clearly evident without sticking fingers up her vagina, she eventually got tired and labour slowed and stopped. She went to bed and I went home. When she woke up, labour resumed and a baby emerged swiftly and joyously. As it turns out, for her, she has a baby after a good sleep with people she trusts.”
What about the routine vaginal exams in late pregnancy? Glad you asked!
Since they don’t have good predictive value, meaning they won’t diagnose when labour will begin, how long it will take, or whether the woman’s pelvis will accommodate that particular baby prior to labour, they have 2 functions.
The first is to plan and initiate your induction.
A cervical exam provides information that is measured against a Bishop Score. A Bishop Score provides a predictive assessment on whether an induction is likely to result in a vaginal birth or is more likely to result in a caesarean for “failure to progress”. A cervix that scores higher is more likely to respond to an induction whereas a lower score indicates a less favourable outcome (25). Further, a vaginal exam allows the practitioner to begin the induction process with a membrane stripping/stretch-and-sweep.
The second purpose for routine vaginal exams in pregnancy is to build in sexual submission. It reaffirms the power dynamic where someone who is not the woman’s intimate sexual partner is allowed to penetrate her genitals at will. It makes their job much simpler once she’s is in labour. She has been trained to accept this violation.
A vaginal exam during labour might rarely be indicated when there is a problem that requires more information. A vaginal exam can help determine if there’s a possible cord prolapse requiring immediate medical attention, or can asses the position and descent of the baby to help suggest strategies to encourage the baby to move into a better position. However, when a labour is spontaneous, meaning it hasn’t been induced by any mechanical, chemical, or “natural” means, the labour isn’t augmented with artificial rupture of membranes or synthetic oxytocin, and the labouring woman is untethered and free to move as her body indicates, complications are far less likely.
Throughout my 35 years in supporting birthing families, I can say that babies do indeed come safely and spontaneously out of vaginas when there’s no one sticking their fingers up there. And they tend to come more quickly. Routine vaginal exams don’t contribute to the safety of the mother/baby. However, they do add to the safety of the practitioner who is tasked with placating the technocratic gods who demand they follow protocols and keep the wheels of the business running on track.
My reasons for not doing vaginal exams, even if the the technocratic gods gave their blessing, include:
They’re rude
They’re unnecessary
They shift the locus of power from the birthing woman to the person with the gloves
They introduce the potential for infection
They interrupt labour and can sabotage a good birth
They often hurt
They can traumatise the cervix
They can traumatise the mother
They can impact the experience of the baby
There are so many simpler ways to determine how labour is progressing
I don’t practice medicine or midwifery or engage in its absurdities
I really am not that interested in other people’s vaginas
Let’s talk about when labour does veer from a normal physiological process.
When the power dynamic places the labouring and birthing mother in charge of the experience, it actually becomes a safer and simpler process. She is the one who is experiencing the labour and birth and is the one relaying information. Only she is in direct communication with her baby. She is the one who knows when labour has exceeded her resources and she needs medical help, pharmacologic pain relief, or the reassurance of the technocratic model.
Of course, not all births unfold simply. However, my experience over these many years is that when women are not expected to submit to exams for the purpose of charting and the subsequent limitations imposed by those charts, birth unfolds a lot more simply far more often.
Much love,
Mother Billie ❤️
Endnotes
Tew, Marjorie. Safer childbirth?: a critical history of maternity care. (2013). Springer.
Garthus-Niegel, S., von Soest, T., Vollrath, M. E., & Eberhard-Gran, M. (2013). The impact of subjective birth experiences on post-traumatic stress symptoms: a longitudinal study. Archives of women's mental health, 16(1), 1-10.
Creedy, D. K., Shochet, I. M., & Horsfall, J. (2000). Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth, 27(2), 104-111.
Schwab, W., Marth, C., & Bergant, A. M. (2012). Post-traumatic stress disorder post partum. Geburtshilfe und Frauenheilkunde, 72(01), 56-63.
Montmasson, H., Bertrand, P., Perrotin, F., & El-Hage, W. (2012). Predictors of postpartum post-traumatic stress disorder in primiparous mothers. Journal de gynecologie, obstetrique et biologie de la reproduction, 41(6), 553-560.
Beck, C. T., Gable, R. K., Sakala, C., & Declercq, E. R. (2011). Posttraumatic stress disorder in new mothers: Results from a two‐stage US National Survey. Birth, 38(3), 216-227.
Shaban, Z., Dolatian, M., Shams, J., Alavi-Majd, H., Mahmoodi, Z., & Sajjadi, H. (2013). Post-traumatic stress disorder (PTSD) following childbirth: prevalence and contributing factors. Iranian Red Crescent Medical Journal, 15(3), 177-182.
Oates, M. (2003). Perinatal psychiatric disorders: a leading cause of maternal morbidity and mortality. British medical bulletin, 67(1), 219-229.
Oates, M. (2003). Suicide: the leading cause of maternal death. The British Journal of Psychiatry, 183(4), 279-281.
Cantwell, R., Clutton-Brock, T., Cooper, G., Dawson, A., Drife, J., Garrod, D., Harper, A., Hulbert, D., Lucas, S., McClure, J. and Millward-Sadler, H. (2011). Saving Mothers' Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG: an international journal of obstetrics and gynaecology, 118, 1-203.
Austin, M. P., Kildea, S., & Sullivan, E. (2007). Maternal mortality and psychiatric morbidity in the perinatal period: challenges and opportunities for prevention in the Australian setting. Medical Journal of Australia, 186(7), 364-367
Palladino, C. L., Singh, V., Campbell, J., Flynn, H., & Gold, K. (2011). Homicide and suicide during the perinatal period: findings from the National Violent Death Reporting System. Obstetrics and gynecology, 118(5), 1056.
Grigoriadis, S., Wilton, A.S., Kurdyak, P.A., Rhodes, A.E., VonderPorten, E.H., Levitt, A., Cheung, A. and Vigod, S.N. (2017). Perinatal suicide in Ontario, Canada: a 15-year population-based study. Cmaj, 189(34), E1085-E1092.
CEMD (Confidential Enquiries into Maternal Deaths) (2001) Why Mothers Die 1997–1999. London: Royal College of Obstetricians and Gynaecologists.
Sareen, J., Cox, B. J., Stein, M. B., Afifi, T. O., Fleet, C., & Asmundson, G. J. (2007). Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic medicine, 69(3), 242-248.
Hudenko, William, Homaifar, Beeta, and Wortzel, Hal. (July 2016). The Relationship Between PTSD and Suicide. PTSD: National Center for PTSD, U.S. Department of Veterans Affair.
Act, Ontario Midwifery. "SO 1991, c. 31." (1991).
Smith Adams, K. L. (1988). From 'the help of grave and modest women' to 'the care of men of sense': the transition from female midwifery to male obstetrics in early modern England. (Master’s thesis, Portland State University.
Burrows, E. G., & Wallace, M. (1998). Gotham: a history of New York City to 1898. Oxford University Press.
Semmelweis, I. (1983). Etiology, concept, and prophylaxis of childbed fever. Carter KC, ed. Madison, WI.
Halberg, F., Smith, H. N., Cornélissen, G., Delmore, P., Schwartzkopff, O., & International BIOCOS Group. (2000). Hurdles to asepsis, universal literacy and chronobiology-all to be overcome. Neuroendocrinology Letters, 21(2), 145-160.
Caughey, A. B., Cahill, A. G., Guise, J. M., Rouse, D. J., & American College of Obstetricians and Gynecologists. (2014). Safe prevention of the primary cesarean delivery. American journal of obstetrics and gynecology, 210(3), 179-193.
Curtin, W. M., Katzman, P. J., Florescue, H., Metlay, L. A., & Ural, S. H. (2015). Intrapartum fever, epidural analgesia and histologic chorioamnionitis. Journal of Perinatology, 35(6), 396-400.
Kauffman, E., Souter, V. L., Katon, J. G., & Sitcov, K. (2016). Cervical dilation on admission in term spontaneous labor and maternal and newborn outcomes. Obstetrics & Gynecology, 127(3), 481-488.
Vrouenraets, F. P., Roumen, F. J., Dehing, C. J., Van den Akker, E. S., Aarts, M. J., & Scheve, E. J. (2005). Bishop score and risk of cesarean delivery after induction of labor in nulliparous women. Obstetrics & Gynecology, 105(4), 690-697.
Beyond the Shot: Preventing Postpartum Haemorrhage ~ Wisdom from a Traditional Birth Companion
Postpartum haemorrhage is a complication that can happen in any birth setting, although it’s more likely in a hospital. Despite the universal application of “active management” as a prevention, the rate of haemorrhage due to uterine atony has been steadily climbing in developed nations.
“Active management of the 3rd stage”, is an intervention for the birth of the placenta, the time when women are most likely to lose a significant amount of blood. It involves injecting the mother with a uterotonic (something to make the uterus contract), usually synthetic oxytocin, as soon as the baby is born, and it may include some other steps like early cord clamping or pulling on the umbilical cord depending on the protocol used. This intervention is applied to all birthing women in all hospitals, birth centres, and homes with few exceptions.
You’d think if every mother everywhere gets this injection, then it must be a good thing. Well, that’s the thing about obstetrics. It tends to take an intervention that might be suitable for some clients in certain situations and applies it to everyone. And the results are increasingly worrisome.
© Billie Harrigan Consulting
“We don’t birth according to the science. We birth according to what we believe.
And we don’t believe the science.”
~ Mother Billie
Hospital-based birth presents some unique safety challenges. Over the years, there have been various efforts to reduce the increased risks. Some of them have been successful, such as hand washing and sanitation to reduce infections, and some of them not at all successful, such as any attempt to reduce unnecessary caesarean sections.
Postpartum haemorrhage is a complication that can happen in any birth setting, although it’s more likely in a hospital (1,2,3,4). Despite the universal application of “active management” as a prevention, the rate of haemorrhage due to uterine atony has been steadily climbing in developed nations (5,6,7,8).
“Active management of the 3rd stage”, is an intervention for the birth of the placenta, the time when women are most likely to lose a significant amount of blood. It involves injecting the mother with a uterotonic (something to make the uterus contract), usually synthetic oxytocin, as soon as the baby is born, and it may include some other steps like early cord clamping or pulling on the umbilical cord depending on the protocol used. This intervention is applied to all birthing women in all hospitals, birth centres, and homes with few exceptions.
You’d think if every mother everywhere gets this injection, then it must be a good thing. Well, that’s the thing about obstetrics. It tends to take an intervention that might be suitable for some clients in certain situations and applies it to everyone. And the results are increasingly worrisome.
To begin – what is a postpartum haemorrhage?
The general definition of postpartum haemorrhage is blood loss of 500mls in the first 24 hours following a vaginal birth, or blood loss of 1000mls following caesarean surgery. A severe postpartum haemorrhage is loss of 1000mls after a vaginal birth (or 1500mls in some locations).
The first question we need to ask is why 500mls was chosen as the threshold for defining a haemorrhage? When no uterotonics are used and postpartum blood loss is measured, the average blood loss in the first hours is actually around 500mls (9,10). Estimating blood loss by looking at it is fairly inaccurate and most observers tend to underestimate blood loss (11,12,13). This means that healthy births that look like they didn’t release much blood have actually released about 500mls in the first hours, which is technically a haemorrhage.
Since 500mls has been selected as the threshold for haemorrhage, the effectiveness of every intervention is based on its ability to reduce the average amount of blood a woman releases in the first hours after birth, because now average is considered pathological.
If we move away from pathologising average amounts of blood, then a new definition of postpartum haemorrhage might be considered. A haemorrhage could be considered as any blood loss that exceeds that mother’s physiological capacity to accommodate it without any accompanying morbidity.
For a mother with adequate iron stores and a healthy blood volume expansion, which is about 1450mls of additional circulating blood, a loss of over 500mls may present no additional challenges. In fact, most women who experience a blood loss of over 500mls receive no clinical intervention or experience any serious consequences (14,15,16). And yet, for a mother who has had a challenging pregnancy or other health concerns, with poor blood volume expansion and exhausted iron stores, a loss of much less might present difficulties and require treatment.
It’s hard to get estimates on the prevalence of postpartum haemorrhages as there are profound differences in reported outcomes from different countries, facilities, and clientele (17). This tells us there are significant differences in how blood loss is measured, the health of the clientele, and what is done to the birthing client that either improves or exacerbates bleeding. And because women are not standardised machines, there is tremendous variability between individuals.
Why does it happen?
About 80% of the time, a postpartum haemorrhage is the result of uterine atony, which is a lack of effective contractions (5,18). Without effective contractions, the blood vessels behind the placenta fail to close and blood continues to flow freely. It can also be caused by physical trauma, for example lacerations in the vagina or cervix from tearing, forceps, or an episiotomy. Uterine rupture can cause a haemorrhage, as can a placental abruption, where the placenta prematurely separates from the uterine wall. Retained placental tissue or blood clotting disorders in the mother can also cause a haemorrhage.
Active management to the rescue!
Active management only addresses uterine atony. It can’t help when the reason for the haemorrhage is physical trauma from tearing or cutting, or address a blood clotting disorder. The World Health Organisation and most medical and midwifery associations recommend giving 100% of women an injection of synthetic oxytocin just after the baby arrives as a means of preventing postpartum haemorrhage (19). Oxytocin is a naturally occurring hormone that causes the uterus to contract. It’s the primary hormone of labour. An injection of 10IU of synthetic oxytocin, either intramuscular or added to an IV, is the recommended intervention. In low resource settings where there is no synthetic oxytocin, which requires stable temperature and a skilled attendant to administer it, then an oral dose of misoprostol is recommended as a preventive.
REX/Shutterstock
What about that shot of synthetic oxytocin?
Synthetic oxytocin is a drug that is marketed under the brand names Pitocin, Syntocinon, and a number of lesser-known brands. It’s a clear aqueous solution that contains a chemically identical synthetic version of naturally-occurring oxytocin. Naturally-occurring oxytocin is produced in the brain by the hypothalamus and released both as a neurotransmitter across the brain facilitating feelings of love, bonding, trust, empathy, and compassion, and as a hormone through the posterior pituitary gland into the blood where it acts on smooth muscles in pulses or waves. Synthetic oxytocin is delivered through a syringe into the mother’s muscle (usually the thigh or bum) or through an IV directly into the blood stream. It does not cross the mother’s blood-brain barrier and doesn’t support bonding with the baby.
Looking at Pitocin, we see that it also contains 0.5% Chlorobutanol, a chloroform derivative as a preservative, acetic acid to adjust its pH, and may contain up to 16% of total impurities (20).
When given as an injection, the uterus responds by contracting within 3-5 minutes and lasts for 2-3 hours. When given in an IV, the uterus responds almost immediately and it lasts about an hour. It’s removed from maternal plasma through the liver and kidneys.
Just like any drug, synthetic oxytocin comes with risks, including
Anaphylactic reaction – an allergic reaction where the individual may stop breathing
Uterine hypertonicity, spasm, or tetanic contraction
Uterine rupture
Premature ventricular contractions – feels like heart palpitations or the heart is “skipping a beat”
Pelvic haematoma – a blood clot similar to a deep bruise
Hypertensive episodes – spiking blood pressure
Cardiac arrhythmia – fluctuations in heartbeat
Nausea and vomiting
Headache, loss of memory, confusion
Loss of coordination, fainting
Seizures
Subarachnoid haemorrhage – bleeding beneath the membrane that covers the brain. This can lead to stroke, seizures, brain damage, and death
Fatal afibrinogenemia – an absence of fibrinogen circulating in the blood which is needed for blood clotting. This leads to sudden and uncontrollable haemorrhage until death
Postpartum haemorrhage
Prolonged bleeding in the days and weeks after birth
“The possibility of increased blood loss and afibrinogenemia should be kept in mind when administering the drug.” ~ drugs.com
The preservative Chlorobutanol has a half-life of 10 days and is anti-diuretic, meaning it will interfere with normal elimination for up to 10 days and may contribute to increased breast engorgement. An allergic reaction can cause dermatitis, usually beginning on the face and chest. It is known to cause light headedness, ataxia (loss of coordination, speech, or eye movement), and nightmares.
Does this intervention work?
The most recent Cochrane Review (2019) (17), reveals that this recommendation is based on studies with “very low” to “moderate” level quality. According to the review, using synthetic oxytocin after the birth of the baby
May reduce the risk of blood loss of 500 mL after delivery (low-quality evidence)
May reduce the risk of blood loss of 1000 mL after delivery (low-quality evidence)
Probably reduces the need for additional uterotonics (moderate-level evidence)
May be no difference in the risk of needing a blood transfusion compared to no intervention (low-quality evidence)
May be associated with an increased risk of a third stage greater than 30 minutes (moderate-quality evidence)
An earlier Cochrane Review revealed that it reduces average blood loss by about 80mls (21). This is usually enough to bring the average blood loss below 500mls thereby avoiding a diagnosis of postpartum haemorrhage. When it comes to severe postpartum haemorrhage of over 1000mls blood loss, it only shows a marginal improvement over expectant management (watching and waiting) (17), and it doesn’t lessen the need for blood transfusion (22).
What else does this drug do?
Synthetic oxytocin dramatically increases the incidence of postpartum depression and anxiety in the first year. In women with a history of depression or anxiety, exposure to this drug increases the risk by a whopping 36%, and for women with no history of depression or anxiety, this drug increases the risk by 32% (23).
Synthetic oxytocin is also associated with greater breastfeeding failure and somatisation symptoms (pain with no known organic cause) (24).
Asking the big questions
Is reducing the average amount of blood loss by about 80mls based on an arbitrary threshold of 500mls worth the risks of this intervention? Are there safer ways to reduce the potential for haemorrhage?
Identifying the risks
There are certain factors that increase the potential for haemorrhage. The rising rates of postpartum haemorrhage have been linked to rising rates of induction and augmentation (25). More women with previous caesareans also mean more haemorrhages, possibly because there are more problems with how the placenta inserts itself in the uterus. Twins or polyhydramnios (excessive water) that overly distends the uterus, is a risk factor. As is pre-eclampsia, chorioamnionitis, and obesity (26).
As mentioned before, hospital birth is a significant risk for a haemorrhage of 1000mls or more (1,2,3,4). This isn’t surprising since hospital births include inductions, augmentations, and complicated pregnancies. However, when comparing the same low risk groups, hospital birth is still an independent risk factor. It’s also the place that is most likely to disrupt the physiology of birth with ritual and routine.
And this is where it gets even more interesting. Studies have shown that when comparing active management with physiological management, that jab of synthetic oxytocin can reduce average blood loss by about 80mls. The problem with these studies is that hospital births are not generally places where physiology is understood or supported. Meaning they might be comparing the same management except that one includes a shot and one doesn’t.
For example, early clamping of the umbilical cord became a world-wide intervention based on terrible presumption and continued in light of great research due to entrenched habit and ego. In one study, women who had a “physiological” 3rd stage had greater postpartum haemorrhages over 1000mls compared to actively managed women (27). The authors noted that the more the placenta weighed, the greater the blood loss. And, why did these placentas weigh so much? Because early clamping of the cord was the usual practice. Draining the cord to reduce the blood volume of the placenta reduces haemorrhage (28) and of course that blood belongs in the baby, not a pail on the floor.
Early cord clamping - Getty Images
In a study where midwives were familiar with the normal birth of the placenta and were less likely to disrupt it, active management doubled haemorrhages over 1000mls (29). In another study where the birth of the placenta was supported with “holistic” care, active management increased the risk of haemorrhage by 7-8-fold (30).
Feeding the mother and the uterus
Labour is an intense activity and requires about 1000 calories of energy per hour. Denying mothers food during labour was an attempt in the 1940’s to prevent her from vomiting under general anesthesia and then breathing in the vomit (31). We know that obstetrics is slow to change, after all, they’ve had 400 years to get women off their backs! Most women are still denied food in a hospital. No one is using the anesthesia of the 1940’s. Forced fasting doesn’t prevent vomiting (32), it only makes the mother more miserable and contributes to a longer labour (33). And longer labours are more likely to be augmented, putting the mother at risk for haemorrhage.
Perhaps a hungry uterus is one that doesn’t contract after the birth of the baby. A study that compared the usual shot of synthetic oxytocin in the mum’s bum to giving her some lovely dates to eat after the birth showed that eating dates was more effective in reducing blood loss than the injection (34). I remember discussing this with some traditional midwives who reported the same great results from giving the mother apricot nectar after the birth. Nourishing mothers is just good care.
© Billie Harrigan Consulting
What is this holistic care that makes birth so much safer?
Holistic care acknowledges that we are mammals and need the same conditions as any mammal giving birth. Birth is a time of reconnection where mother and baby’s interdependence moves from womb to arms. Both the mother and the baby have been waiting for this moment to gaze into each other’s eyes and to say “I know you”. Supporting this reconnection is key to ensuring the birth of the placenta unfolds safely.
And we return to oxytocin, the kind our brain produces, to ensure this reconnection is joyous and safe. Oxytocin is the hormone of love, bonding, trust, empathy, and the one that contracts the uterus and ejects the milk. Oxytocin is also the hormone of orgasms. Anything that disrupts a good orgasm is what disrupts the bonding and the expulsion of the placenta.
Oxytocin is easily encouraged, but it’s also easily disrupted.
holistic care
The room is warm, dimly lit, a sanctuary encircling the mother with love and support. She is nourished and feels safe and cared for. Her labour has begun spontaneously, no drugs, no stretch-and-sweep, and no “natural” induction. The hormones of birth are primed and mother and baby are prepared for this transition from womb to arms. Their hearts cry out for each other; their very skin crawling in anticipation of each other’s touch. The mother heeds the calls of her labour and sways, groans, rises, and pushes. The baby emerges with its protective coating of vernix and is colonised by its mother’s flora. The mother’s waiting hands draw her baby up to her chest which has already adjusted its temperature to ensure the baby is kept warm through her own bodily heat and skin-to-skin contact. The baby smells divine! Its head is releasing pheromones drawn in with each of the mother’s breaths. This baby’s scent reaches the olfactory bulb in the limbic system where the amygdala creates a permanent memory of this precious child. The hypothalamus receives the message that the newest member of our humanity is earthside and sends a gush of oxytocin to ensure bonding, preparation for breastfeeding, and a message to the uterus to contract to begin expelling the placenta. As mother and baby continue to explore each other, the placenta is released and mother feels the urge to expel it. She moves freely, adjusting, and rising to use gravity to her advantage again as it falls gently into a bowl. The bowl is placed next to her as there’s no rush to sever the connection between the baby and its placenta until baby is secure in its connection to its mother. Then she rests, with her baby nestled between her breasts, beginning its journey to her nipple to receive the long-awaited nectar. Both are wrapped in a blanket to ensure they are warm and cocooned. A cup of warm sweet tea and a snack is brought to her and she admires her courage, her strength, and her baby at her breast. Her uterus contracts as it is nourished and charged by the suckling of the baby. Her bleeding is much like a heavy period for a few days, then lessens, and is generally finished within 2-3 weeks.
BSIP/Getty Images
usual care
The room is cool and bright, smelling of antiseptic, the shoes of exhausted nurses and midwives, and echoing the cries of others down the hall. The mother is lying on a narrow bed thrashing as the waves hit, unable to get up, run, leave. The belts are wrapped around her belly measuring each wave requiring her to limit her movement to meet their unfeeling demands. She is exposed and hungry with an IV feeding her fluids and keeping an open port in anticipation of an emergency. On her back, her waves are met with instructions to pull back her legs, bow her head, and hold her breath and push to the count of ten as the room fills with strangers, lights point at her vulva, and the appointed one sits between her legs. The resuscitation station has been warmed and primed to receive her newly born baby. The appointed one may choose to cut open her perineum. As the baby emerges, it is received by the appointed one who may also choose to separate the baby from its source of blood and oxygen through careless ritual. The mother is injected with a dangerous drug and the baby is dried. A hat is placed on the baby’s head so the glory of its scent cannot reach the mother’s limbic system to register this new life. The baby may be wrapped up, preventing the benefits of skin-to-skin, including colonising the mother’s flora, regulating its temperature, and preventing postpartum haemorrhage (35). The baby may be placed on its mother’s chest or it may go to the warming station for weighing and injecting. Once on its mother’s chest, strange hands continue to probe, measure, and instruct. In time, there is food. Her bleeding remains heavy for the first 2 weeks and tends to finish by her 6-week postpartum check-up.
Image by Engin Akyurt from Pixabay
But, but … the hat!
Since the placing of hat is a ritual that is often replicated at home, thereby increasing the potential for haemorrhage, let’s talk some more about it.
Newborn babies don’t regulate their body temperature with the same efficiency as adults. They need help in staying warm. However, biology is glorious and rarely needs our routines. The space between the mother’s breasts adjusts its temperature to ensure the baby is kept at the right temperature, even accommodating the different needs of twins (36). This requires skin-to-skin contact. The other regulating factor is the temperature of the room. A warm room keeps the baby warm (37).
It’s believed that because babies have large heads, they are more likely to lose heat through their heads, so putting a hat on it will keep the baby warm. Only it doesn’t. Stockinette hats don’t affect the core temperature of the baby (38,39). Thermal hats do, and they’re an important part of caring for and transporting a vulnerable premature baby. The only thing knitted hats do is prevent the mother from breathing in the baby’s scent and releasing more oxytocin in response. It’s a foolish ritual.
The elements of holistic care:
Wait for spontaneous labour where possible
Freedom of movement throughout labour to avoid a long labour and augmentation
Nourish the mother with food and drink according to her preference
Warmth and privacy
Spontaneous pushing in the mother’s preferred position
No clamping or cutting of the cord until the placenta is birthed
Immediate skin-to-skin
No hat on the baby
Quiet, private, and supported time between mother and baby
Placenta is birthed by maternal effort aided by gravity
Nourishment for the mother soon after the birth
Ongoing comfort, warmth, and autonomy for the mother
Conclusion
Active management appears to be a dubious and somewhat dangerous intervention that was introduced to overcome obstetrics’ lack of understanding of physiology and their pathological need to disrupt it.
When birth is supported with holistic care, it’s up to 7-8 times safer than routine hospital care with the routine jab. Preventing postpartum haemorrhage comes down to understanding and respecting the physiology of birth, the intense need that mothers and babies have for one another, and not getting in the way. And if there’s a problem, then it requires prompt treatment, but not before to cause the problem.
Much love,
Mother Billie
Endnotes
Scarf, V.L., Rossiter, C., Vedam, S., Dahlen, H.G., Ellwood, D., Forster, D., Foureur, M.J., McLachlan, H., Oats, J., Sibbritt, D. & Thornton, C. (2018). Maternal and perinatal outcomes by planned place of birth among women with low-risk pregnancies in high-income countries: a systematic review and meta-analysis. Midwifery, 62, 240-255.
Hutton, E. K., Cappelletti, A., Reitsma, A. H., Simioni, J., Horne, J., McGregor, C., & Ahmed, R. J. (2016). Outcomes associated with planned place of birth among women with low-risk pregnancies. Cmaj, 188(5), E80-E90.
Blixa, E., Huitfeldtb, A. S., Øiand, P., Straumea, B., & Kumle, M. (2014). Outcomes of planned home births and planned hospital births in low-risk women in Norway between 1990 and 2007: A retrospective cohort study. Sexual & Reproductive Healthcare. Volume 3, Issue 4, December 2012, Pages 147–153.
Nove, A., Berrington, A., & Matthews, Z. (2012). Comparing the odds of postpartum haemorrhage in planned home birth against planned hospital birth: results of an observational study of over 500,000 maternities in the UK. BMC pregnancy and childbirth, 12(1), 130.
Lutomski, J., Byrne, B., Devane, D., & Greene, R. (2012). Increasing trends in atonic postpartum haemorrhage in Ireland: An 11-year population-based cohort study. BJOG: An International Journal of Obstetrics & Gynaecology, 119(3), 306-314.
Callaghan, W. M., Kuklina, E. V., & Berg, C. J. (2010). Trends in postpartum hemorrhage: United States, 1994–2006. American journal of obstetrics and gynecology, 202(4), 353-e1.
Knight, M., Callaghan, W.M., Berg, C., Alexander, S., Bouvier-Colle, M.H., Ford, J.B., Joseph, K.S., Lewis, G., Liston, R.M., Roberts, C.L. & Oats, J. (2009). Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International Postpartum Hemorrhage Collaborative Group. BMC pregnancy and childbirth, 9(1), 55.
Roberts, C. L., Ford, J. B., Algert, C. S., Bell, J. C., Simpson, J. M., & Morris, J. M. (2009). Trends in adverse maternal outcomes during childbirth: a population-based study of severe maternal morbidity. BMC pregnancy and childbirth, 9(1), 7.
Nordström, L., Fogelstam, K., Fridman, G., Larsson, A., & Rydhstroem, H. (1997). Routine oxytocin in the third stage of labour: a placebo controlled randomised trial. BJOG: An International Journal of Obstetrics & Gynaecology, 104(7), 781-786.
Prichard, J. A., Baldwin, R. M., Dickey, J. C., & Wiggins, K. M. (1962). Blood volume changes in pregnancy and the puerperium. Am J Obstet Gynecol, 84, 1271-1282.
Prichard, J. A., Baldwin, R. M., Dickey, J. C., & Wiggins, K. M. (1962). Blood volume changes in pregnancy and the puerperium. Am J Obstet Gynecol, 84, 1271-1282.
Bloomfield, T. H., & Gordon, H. (1990). Reaction to blood loss at delivery. Journal of Obstetrics and Gynaecology, 10(sup2), S13-S16.
Prasertcharoensuk, W., Swadpanich, U., & Lumbiganon, P. (2000). Accuracy of the blood loss estimation in the third stage of labor. International Journal of Gynecology & Obstetrics, 71(1), 69-70.
Carroli, G., Cuesta, C., Abalos, E., & Gulmezoglu, A. M. (2008). Epidemiology of postpartum haemorrhage: a systematic review. Best practice & research Clinical obstetrics & gynaecology, 22(6), 999-1012.
Selo-Ojeme, D. O. (2002). Primary postpartum haemorrhage. Journal of Obstetrics and Gynaecology, 22(5), 463-469.
Prendiville, W. J., Harding, J. E., Elbourne, D. R., & Stirrat, G. M. (1988). The Bristol third stage trial: active versus physiological management of third stage of labour. Bmj, 297(6659), 1295-1300.
Salati, J. A., Leathersich, S. J., Williams, M. J., Cuthbert, A., & Tolosa, J. E. (2019). Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage. Cochrane Database of Systematic Reviews, (4).
Bateman, B. T., Berman, M. F., Riley, L. E., & Leffert, L. R. (2010). The epidemiology of postpartum hemorrhage in a large, nationwide sample of deliveries. Anesthesia & Analgesia, 110(5), 1368-1373.
World Health Organization. (2012). WHO recommendations for the prevention and treatment of postpartum haemorrhage. World Health Organization.
Drugs.com. Retrieved from https://www.drugs.com/pro/pitocin.html April 10, 2020.
Prendiville, W. J., Elbourne, D., & McDonald, S. J. (2000). Active versus expectant management in the third stage of labour. Cochrane database of systematic reviews, (3).
Sloan, N. L., Durocher, J., Aldrich, T., Blum, J., & Winikoff, B. (2010). What measured blood loss tells us about postpartum bleeding: a systematic review. BJOG: An International Journal of Obstetrics & Gynaecology, 117(7), 788-800.
Kroll‐Desrosiers, A. R., Nephew, B. C., Babb, J. A., Guilarte‐Walker, Y., Moore Simas, T. A., & Deligiannidis, K. M. (2017). Association of peripartum synthetic oxytocin administration and depressive and anxiety disorders within the first postpartum year. Depression and anxiety, 34(2), 137-146.
Gu, V., Feeley, N., Gold, I., Hayton, B., Robins, S., Mackinnon, A., Samuel, S., Carter, C.S. & Zelkowitz, P. (2016). Intrapartum synthetic oxytocin and its effects on maternal well‐being at 2 months postpartum. Birth, 43(1), 28-35.
Kramer, M. S., Dahhou, M., Vallerand, D., Liston, R., & Joseph, K. S. (2011). Risk factors for postpartum hemorrhage: can we explain the recent temporal increase?. Journal of Obstetrics and Gynaecology Canada, 33(8), 810-819.
Wetta, L. A., Szychowski, J. M., Seals, S., Mancuso, M. S., Biggio, J. R., & Tita, A. T. (2013). Risk factors for uterine atony/postpartum hemorrhage requiring treatment after vaginal delivery. American journal of obstetrics and gynecology, 209(1), 51-e1.
Jangsten, E., Mattsson, L. Å., Lyckestam, I., Hellström, A. L., & Berg, M. (2011). A comparison of active management and expectant management of the third stage of labour: a Swedish randomised controlled trial. BJOG: An International Journal of Obstetrics & Gynaecology, 118(3), 362-369.
Mohamed, A., Bayoumy, H. A., Abou-Gamrah, A. A. S., & El-Shahawy, A. A. S. (2017). Placental cord drainage versus no placental drainage in the management of third stage of labour: Randomized controlled trial. The Egyptian Journal of Hospital Medicine, 68(1), 1042-1048.
Davis, D., Baddock, S., Pairman, S., Hunter, M., Benn, C., Anderson, J., Dixon, L. & Herbison, P. (2016). Risk of severe postpartum hemorrhage in low-risk childbearing women in new zealand: exploring the effect of place of birth and comparing third stage management of labor-Birth (Berkeley, Calif.)-Vol. 39, 2-ISBN: 1523-536X-p. 98-105.
Fahy, K., Hastie, C., Bisits, A., Marsh, C., Smith, L., & Saxton, A. (2010). Holistic physiological care compared with active management of the third stage of labour for women at low risk of postpartum haemorrhage: a cohort study. Women and Birth, 23(4), 146-152.
Mendelson, C. L. (1946). The aspiration of stomach contents into the lungs during obstetric anesthesia. Obstetrical & Gynecological Survey, 1(6), 837-839.
Ludka, L. M., & Roberts, C. C. (1993). Eating and drinking in labor: a literature review. Journal of Nurse-Midwifery, 38(4), 199-207.
Rahmani, R., Khakbazan, Z., Yavari, P., Granmayeh, M., & Yavari, L. (2012). Effect of oral carbohydrate intake on labor progress: randomized controlled trial. Iranian journal of public health, 41(11), 59.
Khadem, N., Sharaphy, A., Latifnejad, R., Hammod, N., & Ibrahimzadeh, S. (2007). Comparing the efficacy of dates and oxytocin in the management of postpartum hemorrhage. Shiraz E-Medical Journal, 8(2), 64-71.
Saxton, A., Fahy, K., Rolfe, M., Skinner, V., & Hastie, C. (2015). Does skin-to-skin contact and breast feeding at birth affect the rate of primary postpartum haemorrhage: Results of a cohort study. Midwifery, 31(11), 1110-1117.
Ludington‐Hoe, S. M., Lewis, T., Morgan, K., Cong, X., Anderson, L., & Reese, S. (2006). Breast and infant temperatures with twins during shared kangaroo care. Journal of Obstetric, Gynecologic & Neonatal Nursing, 35(2), 223-231.
Perlman, J., & Kjaer, K. (2016). Neonatal and maternal temperature regulation during and after delivery. Anesthesia & Analgesia, 123(1), 168-172.
De Saintonge, D. C., Cross, K. W., Shathorn, M. K., Lewis, S. R., & Stothers, J. K. (1979). Hats for the newborn infant. Br Med J, 2(6190), 570-571.
Coles, E. C., & Valman, H. B. (1979). Hats for the newborn infant. British medical journal, 2(6192), 734.
The Art of Palpation ~ Wisdom from a Traditional Birth Companion
Palpation is the act of using one’s hands to figure out something on or in a body. In maternity services, the practitioner routinely palpates the pregnant belly to assess the position and size of the foetus.
After the male midwife, which later became the obstetrician, infiltrated birth services and paternalized it into a male-centric, provider-centric practice, they’ve been “discovering” all kinds of things that were just normally known and carried out by midwives for centuries. Among them is the standard way to palpate a pregnant belly.
I tend to see palpation through a different lens. I feel it’s more about building a relationship with the baby than anything else.
Nana playing with/palpating her granddaughter before she was born. ©Billie Harrigan Consulting
Palpation is the act of using one’s hands to figure out something on or in a body. In maternity services, the practitioner routinely palpates the pregnant belly to assess the position and size of the foetus.
After the male midwife, which later became the obstetrician, infiltrated birth services and paternalized it into a male-centric, provider-centric practice, they’ve been “discovering” all kinds of things that were just normally known and carried out by midwives for centuries. Among them is the standard way to palpate a pregnant belly.
German obstetrician-gynaecologist Christian Gerhard Leopold (1846-1911) is credited with the obstetrical manoeuvre used today to palpate pregnant bellies called ‘Leopold’s Manoeuvre’.
Leopold’s Manoeuvre is a series of 4 specific actions. These 4 actions, along with an assessment of the maternal pelvic shape will help the practitioner to determine if complications will occur during delivery and whether a caesarean should be recommended. They think of it much like a crystal ball that somehow predicts the future. In the provider-centric world of maternity services, it’s another way the practitioner replaces the pregnant mother as the expert on her body and her birth and minimises the power of the birth dance where the mother and baby work together through movement to bring the baby earthside.
Manoeuvre one: Fundal Grip
The practitioner walks their hands up the sides of the uterus to the top of the uterus, called the ‘fundus’. Palpating the upper abdomen will determine if the foetus is lying longitudinal (up/down), oblique (on an angle), or transverse (side-to-side). If the baby is longitudinal, palpating the upper abdomen should determine if it’s a bum or a head.
Manoeuvre two: Umbilical Grip
Next is to determine where the foetal back is lying. By placing hands on either side of the mid-abdomen, the practitioner applies deep pressure on alternating sides to determine where the back is and where the extremities are (arms and legs).
Leopold’s Manoeuvres - public domain
Manoeuvre three: Pawlick’s Grip
This is also named after a male obstetrician-gynaecologist, Karel Pawlick (1849-1914). This step determines how much of the foetus is above the pelvic inlet. The practitioner uses their fingers and thumb to grasp the lower abdomen, just above the pubic bone (pubic symphysis) to feel how much of the foetus can be felt above the pubic bone.
Manoeuvre four: Pelvic Grip
The practitioner faces the patient’s feet and tries to locate the foetus’ brow by placing both hands on the lower abdomen and moving the fingers of both hands towards the pubis by sliding the hands over the sides of the patient’s uterus. On the side where there is the greatest resistance to the practitioner’s descending fingers is the baby’s brow. A well-flexed head, meaning the chin is tucked down towards the chest, will be on the opposite side of the foetal back. If the head is extended, that is, looking straight ahead or upwards, the back of the head is felt on the same side where the back was found. If the brow cannot be found, the head is descended into the pelvis.
With the routine overuse of ultrasound, many practitioners are losing the art of palpation. Routine multiple ultrasounds are now taking the place of non-invasive and non-risky palpation to assess foetal size (with varying degrees of accuracy), amniotic fluid volume (with varying degrees of accuracy), and position of the baby (with a great deal of accuracy). It could be that since ultrasound is very accurate at determining position, practitioners are losing confidence in their own skills.
As a Traditional Birth Attendant, I like palpating pregnant bellies. I especially like it as a grandmother (Nana). Nothing delights me more than playing with my own grandchildren inside their mother’s bellies. In fact, Nana has turned her own grandchild from breech to cephalic. It’s a simple skill that tends to make me a more useful grandmother.
In all the texts I scoured that discusses how to do Leopold’s Manoeuvre, not once was the foetus ever considered as a sentient member of the procedure. The mother’s comfort is often considered, but primarily, it’s about the practitioner doing something to the client to gather information.
I tend to see palpation through a different lens. I feel it’s more about building a relationship with the baby than anything else. After all, if I’m going to be invited to the birth, the baby should know who I am and whether I am someone they can trust to care for their mummy and therefore take care of them.
In my relationship with pregnant families, the first part of palpating a pregnant belly is to ask the mother if she would like this. She doesn’t have to submit to this. This is her choice. I’ve had clients with a history of sexual assault where this was a very threatening idea that someone would be touching their belly and never wanted it. Instead, they just told us where the baby was and what their guess was on how big the baby was. As it turns out, maternal guessing is pretty accurate and often beats the guesses of ultrasounds or experienced practitioners (1). Another client liked palpation, but could only do it sitting up with one hand over her breasts and one protecting her groin.
If the mother agrees to palpation, then I always suggest she go relieve her bladder first. There’s nothing worse than someone playing with your belly and a full bladder. It’s a recipe for leaking out a wee drip or a pent-up fart.
I have a nice couch by a sunny window that clients are invited to lie down on with as many pillows behind them as feels comfortable. I tend to sit on the couch with them nestled beside their legs.
Now here comes the most important part of palpation:
I introduce myself to the baby.
I say hello to the baby. I tell them my name and that I’m a friend of their mummy and daddy. I let them know that Nana often has cold hands.
I start very gently and talk to the baby the whole time. There are no pre-determined set of manoeuvres as this is usually led by the baby. I may find their little bum and squeal with delight! I talk about how much they’re growing. I invite them to play with me. Sometimes their little foot will poke out to start a little game with me. I’ll ask them to show me what position they’re in and if they’d be ok with us listening to their heartbeat with a fetoscope. If my hands are going to go lower on the mother’s abdomen to where a head might be nestled, I always ask permission from the mother before touching her anywhere close to her pubic bone. Likewise, if the parents want a measurement of fundal height, it’s the mother that places the end of the measuring tape on the top of her pubic bone. There’s no need for someone else to be rooting around down there. Once mum picks her spot where the tape measure starts, then that also helps to eliminate measuring errors that can come with multiple people measuring her belly and placing the tape differently.
Some babies become quite playful. And some will lie quietly, listening to me, deciding if I am friend or foe. It becomes quite easy to sense the baby’s receptivity. A baby who has taken a journey along with their mother through previous obstetric mistreatment or disrespectful prenatal visits will often lie quietly, perhaps taking in their mother’s reactions. It may take another visit to warm up to me and become more playful. I tell them that by the time they arrive, I hope we’ll be good friends.
Through gentle palpation, the baby and I are getting to know each other. The parents and I are building trust. We’re having fun! And through gentle touch, we discover where the baby is positioned at that particular moment. It’s not predictive of much else. Even persistently breech babies have turned in labour when I’ve been present. Perhaps in the presence of calm and loving family and birth attendant, the babies felt it a simple matter to rotate and come out head first.
Through gentle palpation, we can also get a sense for how much amniotic fluid is in the womb. It’s a chance to talk about hydration and salt. Parents are invited to listen to their baby’s heartbeat with a fetoscope, and depending on the position of the placenta, they may be treated to the sounds of its ‘whooshing’ as blood flows through the maternal side.
A fetoscope is non-invasive and listens to the baby’s heartbeat and the placenta
Through gentle palpation, we can invite the baby to adjust their position to make it easier on mummy. Perhaps a poking foot is feeling like it’s about to break mummy’s rib. Or little one hasn’t started the descent down into the pelvis as it gets closer to term. Having a simple conversation with the little one and explaining how they can help has shown over and over that these precious babies are sentient and love their mothers and want to participate in a loving and safe arrival.
And to conclude the palpation, I thank the baby for allowing me to play with them.
This gentle approach has brought many mothers to tears. For many of them, it’s the first time their body and their baby have been treated with reverence. In fact, I too, have often been brought to tears by the enthusiastic response of these precious babies who quickly understand that I care deeply about them.
Modern maternity services are decidedly centred around the practitioner. The manoeuvres designed to gather information help the practitioner to determine a course of action that lessens the potential for an obstetrically-determined negative outcome. However, truly client-centred and family-centred maternity care includes the baby as a fully sentient member of the family who deserves as much care, caution, respect, and dignity as every other member of the family. And that’s where we see some of the best outcomes!
Much love,
Mother Billie
©Billie Harrigan Consulting
Endnote
1. Ashrafganjooei, T., Naderi, T., Eshrati, B., & Babapoor, N. (2010). Accuracy of ultrasound, clinical and maternal estimates of birth weight in term women. EMHJ-Eastern Mediterranean Health Journal, 16 (3), 313-317, 2010.
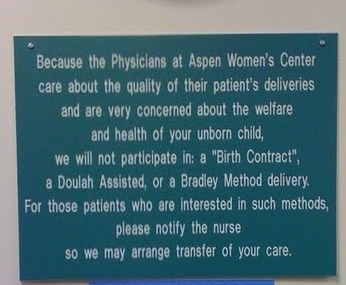
Appeasing the Patriarchy
Recently, the Association of Ontario Doulas (AOD) released their Statement of Position on Non-Aboriginal Traditional Birth Attendant/Companion (TBC) (January 15, 2024) that you can read by following this link.
Since it is a position that is directed at my work in creating and defining the role of a traditional birth companion, it warrants a response.
Content note: This Statement of Position uses sex-based language. The word ‘women’ is used in its historical and traditional context to mean that half of our species that arrives with the biological potential to ovulate, menstruate, conceive, gestate, birth, and lactate. By continuing to read this post you agree to be entirely responsible for your own reactions and your emotional, psychological, and intellectual well-being and hold us free from liability for use of this word.
Billie: of the family Harrigan, elder and companion, Statement of Position re: the Association of Ontario Doulas’ Statement of Position on Non-Aboriginal Traditional Birth Attendant/Companion (TBC)
Whereas the Association of Ontario Doulas (AOD) has released their statement of position regarding non-aboriginal traditional birth attendants/companions that directly misrepresents this emerging sovereign alternative that is spearheaded by me and my efforts, I, Billie: of the family Harrigan offer my commentary and position on their position.
It arrives unsurprisingly, and reads as submissive pandering to existing patriarchal power structures that are both collapsing and increasingly detrimental to the wellbeing of the women who use these services and their babies. It’s filled with innuendo and suggestion that is perhaps meant to intimidate their members into ongoing conformity and obedience.
Since I am the one who has created the unique role of a traditional birth companion in Canada and beyond and I am the one who gave it that name, I am the one who defines it. Not the AOD. Their misrepresentation of my work is stunning. However, it may fit with my hypothesis that the doula profession is limited in its maturation by their alarmingly high and early burnout. Wisdom and insight require time and perseverance.
Prior to the push to move women into hospitals after WW2, it was the tradition in Canada for most women to simply call the neighbour who had some birth skills and experience. This neighbourly support did not include the medical surveillance and interventions associated with modern midwifery. Traditional birth attending or companioning did not have the tools nor the religious-like zeal to engage in today’s fear-based management of a common physiological experience.
Whilst a TBA has “historically referred to indigenous midwives, lay midwives, and community midwives”, a TBC is an invention of mine based on my own 40 years of experience as a companion (as I define it) and my work as an academic specialising in maternity care. Further, traditional midwifery, as that which was practiced prior to the fairly recent medicalisation of childbirth, in no way resembled what passes for midwifery today. The AOD is conflating practices from different eras by using ‘historical’ to define this role and inserting modern medical regulation & practices to suggest they are operating in tandem.
The historical role of the TBA has been largely eliminated by that great coloniser, the WHO and its unholy alliance with pharma and their money in favour of the western medical model as created by Rockefeller and Carnegie. Actual traditional practices have been replaced with modern interventions based on our current cultural belief in the supposed perils of women’s physiology. To suggest a TBC engages in these modern medical practices, as opposed to historical (traditional), non-medical, and un-controlled offerings is to incite division through misrepresentation.
Their statement included the medical industry’s response to women’s choices to leave these services. It’s expected that any industry with a monopoly that is losing control will come out with some statement about how their former customers are being foolish or dangerous. It’s just another example of their suffocating paternalism. The AOD would benefit from reflecting carefully on why they too participated in this paternalism.
It was a curious statement that licensed medical practitioners “are the only ones authorized to ‘practice spontaneous childbirth’” as women all over the earth are releasing their babies in a practice of spontaneous childbirth without any authorisation whatsoever.
It should be noted and carefully understood that the “risk that child welfare organisations may investigate” comes ONLY from another human who calls this agency for an investigation. This human is overwhelmingly a licensed medical practitioner who takes exception that the customer, who arrives to access their services, did not use their services prior to needing their services. It’s a well-documented terror tactic in the realm of obstetric violence that is designed to send a message that families will be punished for non-compliance. It comes from deeply rooted medical narcissism, cult-like behaviour and belief in their offerings, and a complete absence of trauma-informed training or skills. It behoves the AOD to take a firm stand against this heinous practice and advocate for families rather than including it as a threat to families who may not acquiesce to medical control over their family decisions. This omission alone disqualifies the AOD from having a voice for medical autonomy in Ontario.
The AOD’s insinuation or assumption that a TBC “manages labour or conducts the delivery of a baby” in contravention to the Controlled Act is an example of organisational ignorance, as no one has actually contacted me to find out what we do. Further, it’s inflammatory and fuels a political agenda that isn’t about women’s health outcomes but rather the AOD’s hopes for a regulated role within Ontario’s massive medical infrastructure.
Their inclusion of “there have been a number of serious incidents, including a death, in which the birther has chosen a non-Indigenous Traditional Birth Attendant/Companion” takes a page from the technocratic medicalised birth services industry’s playbook that excessively threatens their clients with a dead baby or a dead mother to gain acquiescence in lieu of informed consent or refusal. It was an abhorrent attempt to implicate non-regulated companions as being directly responsible for an adverse outcome. Given the extreme circumstances of the last few years, there have been an exorbitant number of serious incidents and deaths. And yet, there was no mention of the rate of adverse outcomes or deaths in the presence of regulated practitioners. The AOD can no longer claim any moral high ground when it comes to denouncing this tactic to bypass consent. They have learned how easy it is to play the ‘dead baby/mother’ card.
It's important to address their vague threat that “Legal entities may confuse individuals operating in this capacity as people working as unlicensed healthcare providers” along with mention of fines and detention. This confusion could be easily eliminated by careful statements that speak the truth. There is no confusion when the role of a TBC, as I have created it, is represented truthfully and accurately.
Their statement declares that “some” Indigenous communities reserve the use of the word “traditional”. Whilst this may be so for some communities, there is no consensus within the English language that limits its use to aboriginal peoples. Instead, it has a broad understanding to mean things that are not new, typical or normal for someone or something, or doing something for a long time for a particular group. The AOD has misappropriated the historical TBA and the current TBC into their political ideology that is an affront to both.
Modern technocratic medical maternity services are the result and technological iteration of Rockefeller medicine that gained a monopoly through the fraudulent Flexner report and oil money. Safer and saner alternatives exist and could be accessed by more families. However, existing power structures enjoy a monopoly and will not yield to women’s sovereignty and their alternatives. The AOD has come out firmly on the side of existing power structures in spite of their devastatingly high adverse outcomes, trauma, and postpartum suicide as a leading cause of maternal mortality. Their allegiance is with historical patriarchy, medical paternalism, and the ongoing bondage of women in childbirth to a medical model that will not change despite any delusion that they will work together with doulas to improve maternal care outcomes.
In fact, if there’s any lingering confusion about the actual position of the AOD, consider that they put out a call for snitches. The witch hunts never did end.
Despite statements like this from organisations who appear to want to appease oppressive systems for potential recognition or ‘credibility’, the real work to improve maternal outcomes is being done by ordinary women who opt for safer solutions so that more babies arrive safely and gently from healthy, empowered, and non-traumatised mothers. They are becoming more useful humans. The AOD misrepresents my work for political gain, but the women carry on. As we always have.
The system isn’t broken - but its people are
One third of birthing parents has a traumatic birth.
“The system is broken.”
One in 8 new parents enters parenthood with postpartum PTSD from the experience.
“The system is broken.”
Depending on where you live, one third, one half, or almost everyone has a surgical birth.
“The system is broken.”
One in 6 women are abused during their births.
“The system is broken.”
If we say it enough, we might believe it. However, the “system” is decidedly NOT broken. It is doing exactly what it was set up to do by any means available to it.
One third of birthing parents has a traumatic birth.[i] [ii] [iii]
“The system is broken.”
One in 8 new parents enters parenthood with postpartum PTSD from the experience.[iv]
“The system is broken.”
Depending on where you live, one third, one half, or almost everyone has a surgical birth.[v]
“The system is broken.”
One in 6 women are abused during their births.[vi]
“The system is broken.”
If we say it enough, we might believe it. However, the “system” is decidedly NOT broken. It is doing exactly what it was set up to do by any means available to it.
The “system” is how we deliver maternity services. It began when male-midwives, those physicians who broke social etiquette, began attending women in birth. They were barbaric in means because they were sanctioned by the Catholic church to carry sharp instruments that women were forbidden to use. Male barber-surgeons, the Chamberlains, invented the forceps but kept their secret hidden for a century. A few centuries of witch hunts where midwives and female healers were persecuted and executed taught the public to shy away from learning these skills – if they were women. The collusion of religion and medicine ensured that men gained and maintained a monopoly over sick care and what women were allowed to do with their own bodies.[vii]
Eventually, through clever marketing, the male midwife became the preferred attendant as they were considered superior in intellect.[viii] [ix] Women were forbidden to attend universities, practice medicine, or serve in leadership in religions that ruled the western politic, thus unable to influence how women were treated in childbirth.[x]
Sure enough, these clever men discovered how much more profitable it was to bring birthing clients to them rather than going out to their homes.[xi] And so emerged the ‘lying-in’ hospital. The wholesale slaughter of women in these death traps was on par with the witch hunts of a few centuries prior. One in ten women died from puerperal fever, brought on by the unwashed hands of physicians who went from cadaver to the birthing vagina.[xii] Despite the protests of the offensive Semmelweis to wash their hands, ego and elitism prevented them from adopting this simple strategy for many more years thus ensuring the needless deaths of countless more women.[xiii]
Ignaz Semmelweis washing hands with chlorine-water, 1846
Once chloroform and other means of anesthesia were available for use in childbirth, the medical societies lobbied the government to grant them exclusive access. Not that they were any more qualified to use these powerful drugs than any other discipline, they merely had the ear of those in power who made these decisions.[xiv] Next followed the most effective smear campaign in all of history to drive midwives and alternative healing modalities out of business. [xv] [xvi] By the end of WW2 the campaign was almost complete. Next came effective lobbying to ensure governments were only favourable to their approach and the money, legislations, and endorsements flowed to hospital based technocratic birth where the obstetrician is royalty.
Even today, midwives around the world are persecuted and legislated out of business for offering client-centred care and serving women outside of hospitals.
Leaning heavily on Henry Ford’s conveyor belt system of turning out cars, optimisations and standardisations were implemented to cut costs, increase revenue, and turn the business of birth into a well-oiled machine.[xvii]
What we have is an effective system of profit for those industry players who set it up this way.
Of course, women are abused in birth! It’s an effective means of getting them to submit to a routine, one-size-fits-all, conveyor belt, in-and-out, profitable baby factory.
Even the current schedule of prenatal visits has no basis in science, evidence, or benefit. It was created by those same male-midwives who took a good thing and made it $tandard. Certainly, diagnosing and treating medical issues is an important healthcare strategy, whether pregnant or not. In light of the evidence that today’s current schedule and routines have not produced the promised results of healthier pregnancies or births, the industry recommended and implemented a strategy to convince the public that the process of pregnancy could not be trusted to stay normal without their surveillance.[xviii]
Now let’s talk about the people.
Some people enter this industry because it’s proven itself as a profitable endeavour. Obstetrics includes a great deal of power and control over a physiological process that in most cases would unfold quite simply without them. This appeals to some people. It’s a position of elitism and sits higher on the social hierarchy. There’s nothing to see there. Nothing to reach. Nothing to change.
And some enter this industry because they believe they have something valuable to offer during one of the most sacred and vulnerable times in a person’s life. They believe in the importance of how new humans are greeted into this world.
But because they have entered a highly successful system, they witness and sometimes participate in horrific abuses of mothers and babies. Some are broken by this and are the walking and working wounded, grappling with trauma, burnout, PTSD, and even suicidal ideation. Some survive and continue doing the best they can without the learned skillset of trauma-informed care that protects them and their clients. And some become part of the system of abuse and profit as their initial purpose is co-opted by internalised patriarchy and misogyny.
But what’s to be done with those who are broken and those who are merely surviving? The system doesn’t care if they burnout and leave. Players are easily replaced by new inductees at beginner salaries. It was never set up to take care of anyone. It was set up as a profitable means of co-opting physiology for profit based on fear and coercion.
“What we have is a medical system that is literally killing people through suicide.”
Break time. Nature and birth are not always kind. Women have always benefited from the companionship and knowledge of their midwives. And when events became problematic, skilled surgeons and expert paediatricians have brought hope and life where there was once only death. This post only speaks to the system of facility-based birth that currently exists within a patriarchal, misogynistic, and technocratic paradigm.
Back to the people.
‘Burnout’ consists of three features
Emotional exhaustion – feeling emotionally depleted from being overworked
Depersonalisation and cynicism – unfeeling towards patients and peers with often negative, callous, and detached responses
Reduced personal efficacy – a reduced sense of competence or achievement in one’s work
Burnout, compassion fatigue, and trauma are often intermingled in the academic literature so it’s hard to get a sense of the enormity of the issue. However, we do know this:
Physicians
Female physicians have higher rates of burnout and less work satisfaction than males[xxiii]
Physicians have the highest rate of suicide of any profession[xxiv]
General population - 12.3 per 100,000
Physicians -28 to 40 per 100,000
Equal numbers of male and female physicians complete a suicide
Midwives
Midwives around the world report rates of burnout from 20%[xxv] to 65%[xxvi]
One third of midwives have clinical PTSD[xxvii]
Witnessing abusive care of patients creates more severe PTSD[xxviii]
Nurses
35% of labour and delivery nurses have moderate to severe secondary traumatic stress[xxix]
Witnessing or participating in abusive births is a direct contributor to trauma
24% higher rate of suicide than those outside the profession[xxx]
Nurses and Midwives
Female 192% more likely to complete suicide than females in other occupations
8.2 per 100,000 vs 2.8 per 100.000
Male 52% more likely to complete suicide than males in other occupations
22.7 per 100,000 vs 14.9 per 100.000
Male 196% more likely to complete suicide than female colleagues
22.7 per 100,000 vs 8.2 per 100.000[xxxi]
Doulas
Half of doulas report burnout[xxxii] where traumatic incidences and witnessing the mistreatment of labouring clients were direct causes of burnout. Secondary trauma causes doulas to leave the profession early, especially in light of institutional hostility, low income, and routine abuses of their clients[xxxiii]
From the client’s perspective, the simple answer is to birth outside the system.[xxxiv] It’s a reasonable option – unless you’ve drunk the Kool Aid and feel these parents are a danger to their foetus and must be punished through disrespectful care[xxxv] and calls to Childrens Apprehension Services. If enough clients choose an alternative to the system, then simple economics will drive change to bring back the customers.
Birthing families are paying a steep price for system-driven birth. High rates of trauma, postpartum PTSD, postpartum depression and anxiety, relationship breakdowns, and postpartum suicide.[xxxvi] [xxxvii] [xxxviii] [xxxix] [xl] [xli] What we have is a medical system that is literally killing people through suicide.
So, what to do with the crippling loss of health and wellness in those professionals who chose to enter the system to support families in a humane and compassionate manner? Is it even possible to bring back those who have lost their way?
Because the system of institutionalised maternity services is predicated on a patriarchal and misogynistic paradigm of control and elitism, it will never take care of those who are on the front lines. We must learn to take care of ourselves and each other.
Many good and decent people entered into the system of technocratic birth services with all the requisite technical skills and a desire to make a difference in the lives of birthing families. What was missing from their education and skills development were those specific skills that would equip them to work in that environment without losing their soul, their identity, or their life.
Fortunately, the same research that identifies the many problems with this delivery system of services, also identifies the many solutions. For those that are on a journey out of trauma and professional burnout towards recovery and professional efficacy, there are proven strategies that can help walk you towards recovery and wholeness. You can learn
A research-based understanding of the causes and consequences of birth trauma in the birthing client and how to avoid participating
A thorough understanding of secondary and vicarious trauma and its effects in healthcare providers
How to build neurological, biological, psychological, social, cultural, and structural resilience
The positive impact of affective empathy and how to use it
How to employ a trauma-informed approach with clients and peers that improves clinical accuracy, client and professional well-being, and reduces burnout, medical mistakes, and litigation
A knowledge of therapeutic modalities that are specific to trauma
Recovery is possible for those who seek it. While the system runs perfectly as it was designed to, it’s also possible that with enough recovered, equipped, and healthy participants we might see some significant changes that actually helps it to live up to its marketing of “healthy baby healthy mother”. In time, it might even include “healthy professionals”.
I’ve got the science. I’ve got the experience. And I’ve got the tools to help. Let’s do this together.
Much love,
Mother Billie
Endnotes
[i] Garthus-Niegel, S., von Soest, T., Vollrath, M. E., & Eberhard-Gran, M. (2013). The impact of subjective birth experiences on post-traumatic stress symptoms: a longitudinal study. Archives of women's mental health, 16(1), 1-10.
[ii] Creedy, D. K., Shochet, I. M., & Horsfall, J. (2000). Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth, 27(2), 104-111.
[iii] Schwab, W., Marth, C., & Bergant, A. M. (2012). Post-traumatic stress disorder post partum. Geburtshilfe und Frauenheilkunde, 72(01), 56-63.
[iv] Montmasson, H., Bertrand, P., Perrotin, F., & El-Hage, W. (2012). Predictors of postpartum post-traumatic stress disorder in primiparous mothers. Journal de gynecologie, obstetrique et biologie de la reproduction, 41(6), 553-560.
[v] Boerma, T., Ronsmans, C., Melesse, D. Y., Barros, A. J., Barros, F. C., Juan, L., ... & Neto, D. D. L. R. (2018). Global epidemiology of use of and disparities in caesarean sections. The Lancet, 392(10155), 1341-1348.
[vi] Vedam, S., Stoll, K., Taiwo, T. K., Rubashkin, N., Cheyney, M., Strauss, N., ... & Schummers, L. (2019). The Giving Voice to Mothers study: inequity and mistreatment during pregnancy and childbirth in the United States. Reproductive health, 16(1), 77.
[vii] Ehrenreich, B., & English, D. (2010). Witches, midwives, & nurses: A history of women healers. The Feminist Press at CUNY.
[viii] Smith Adams, K. L. (1988). From 'the help of grave and modest women' to 'the care of men of sense': the transition from female midwifery to male obstetrics in early modern England. (Master’s thesis, Portland State University.
[ix] Burrows, E. G., & Wallace, M. (1998). Gotham: a history of New York City to 1898. Oxford University Press.
[x] Minkowski, W. L. (1992). Women healers of the middle ages: selected aspects of their history. American journal of public health, 82(2), 288-295.
[xi] Tew, M. (2013). Safer childbirth?: a critical history of maternity care. Springer.
[xii] Loudon, I. (2000). The tragedy of childbed fever. New York, Oxford University Press.
[xiii] Tew, M. 2013, op. cit.
[xiv] Bonner, T. N. (1989). Abraham Flexner as critic of British and Continental medical education. Medical history, 33(4), 472-479.
[xv] Getzendanner, S. (1988). Permanent injunction order against AMA. JAMA, 259(1), 81-82.
[xvi] Weeks, John. (n.d.). “AMA ‘Thwarts’ Other Professions Practice Expansion and a Challenge to CAM-IM Fields”. The Integrator Blog. http://theintegratorblog.com/?option=com_content&task=view&id=73&Itemid=1
[xvii] Perkins, B. B. (2004). The medical delivery business: Health reform, childbirth, and the economic order. Rutgers University Press.
[xviii] Ball, J. (1993). The Winterton report: difficulties of implementation. British Journal of Midwifery, 1(4), 183-185.
[xix] Peckham, C. (2016). Medscape lifestyle report 2016: bias and burnout. New York, NY: Medscape.
[xx] Avery, Granger, M.D., (2017). The role of the CMA in physician health and wellness. Canadian Medical Association.
[xxi] Imo, U. O. (2017). Burnout and psychiatric morbidity among doctors in the UK: a systematic literature review of prevalence and associated factors. BJPsych bulletin, 41(4), 197-204.
[xxii] Wu, F., Ireland, M., Hafekost, K., & Lawrence, D. (2013). National mental health survey of doctors and medical students.
[xxiii] Peckham, C., 2016, op. cit.
[xxiv] T’Sarumi, O., Ashraf, A., & Tanwar, D. (2018). Physician suicide: a silent epidemic. Reunión Anual de la American Psychiatric Association (APA). Nueva York, Estados Unidos, 1-227.
[xxv] Henriksen, L., & Lukasse, M. (2016). Burnout among Norwegian midwives and the contribution of personal and work-related factors: a cross-sectional study. Sexual & Reproductive Healthcare, 9, 42-47.
[xxvi] Creedy, D. K., Sidebotham, M., Gamble, J., Pallant, J., & Fenwick, J. (2017). Prevalence of burnout, depression, anxiety and stress in Australian midwives: a cross-sectional survey. BMC pregnancy and childbirth, 17(1), 13.
[xxvii] Sheen, K., Spiby, H., & Slade, P. (2015). Exposure to traumatic perinatal experiences and posttraumatic stress symptoms in midwives: prevalence and association with burnout. International journal of nursing studies, 52(2), 578-587.
[xxviii] Leinweber, J., Creedy, D. K., Rowe, H., & Gamble, J. (2017). Responses to birth trauma and prevalence of posttraumatic stress among Australian midwives. Women and birth, 30(1), 40-45.
[xxix] Beck, C. T., & Gable, R. K. (2012). A mixed methods study of secondary traumatic stress in labor and delivery nurses. Journal of Obstetric, Gynecologic & Neonatal Nursing, 41(6), 747-760.
[xxx] Office for National Statistics. (2017). Suicide by occupation, England: 2011 to 2015.
[xxxi] Milner, A.J., Maheen, H., Bismark, M.M., & Spittal, M.J. (2016) Suicide by health professionals: a retrospective mortality study in Australia, 2001–2012. Medical Journal of Australia 205 (6): 260-265.
[xxxii] Naiman-Sessions, M., Henley, M. M., & Roth, L. M. (2017). Bearing the burden of care: emotional burnout among maternity support workers. In Health and Health Care Concerns Among Women and Racial and Ethnic Minorities (pp. 99-125). Emerald Publishing Limited.
[xxxiii] Roth, L. M., Heidbreder, N., Henley, M. M., Marek, M., Naiman-Sessions, M., Torres, J. M., & Morton, C. H. (2014). Maternity support survey: A report on the cross-national survey of doulas, childbirth educators and labor and delivery nurses in the United States and Canada.
[xxxiv] Holten, L., & de Miranda, E. (2016). Women׳ s motivations for having unassisted childbirth or high-risk homebirth: An exploration of the literature on ‘birthing outside the system’. Midwifery, 38, 55-62.
[xxxv] Vedam, S., Stoll, K., Rubashkin, N., Martin, K., Miller-Vedam, Z., Hayes-Klein, H., & Jolicoeur, G. (2017). The Mothers on Respect (MOR) index: measuring quality, safety, and human rights in childbirth. SSM-Population Health, 3, 201-210.
[xxxvi] Oates, M. (2003). Perinatal psychiatric disorders: a leading cause of maternal morbidity and mortality. British medical bulletin, 67(1), 219-229.
[xxxvii] Oates, M. (2003). Suicide: the leading cause of maternal death. The British Journal of Psychiatry, 183(4), 279-281.
[xxxviii] Lewis, G. (2007). Saving mothers' lives: reviewing maternal deaths to make motherhood safer 2003-2005: the seventh report of the confidential enquiries into maternal deaths in the United Kingdom. CEMACH.
[xxxix] Austin, M. P., Kildea, S., & Sullivan, E. (2007). Maternal mortality and psychiatric morbidity in the perinatal period: challenges and opportunities for prevention in the Australian setting. Medical Journal of Australia, 186(7), 364-367.
[xl] Palladino, C. L., Singh, V., Campbell, J., Flynn, H., & Gold, K. (2011). Homicide and suicide during the perinatal period: findings from the National Violent Death Reporting System. Obstetrics and gynecology, 118(5), 1056.
[xli] Grigoriadis, S., Wilton, A. S., Kurdyak, P. A., Rhodes, A. E., VonderPorten, E. H., Levitt, A., ... & Vigod, S. N. (2017). Perinatal suicide in Ontario, Canada: a 15-year population-based study. Cmaj, 189(34), E1085-E1092.
Birth Hijacked – The Ritual Membrane Sweep
I’ve written about many topics over the years but nothing has ever generated as much discussion, opposition, and vitriol as challenging the cherished routine membrane sweep/stripping, aka stretch-and-sweep. A few years ago, I wrote a post about how I’d like to see the routine, prior-to-40-weeks, without-medical-indication membrane sweep banned from obstetrical and midwifery practice. I talked about its risks and the fact that the clients I worked with called it a sexual assault when done without consent
The post went viral and I received hate messages and emails from around the world defending this procedure. In general, the sentiment was that I should most definitely be having sexual relations with myself, after which, I should be locked up and forever silenced. I also heard from hundreds of women whose births were ruined by days of painful, non-progressing contractions triggered by a membrane sweep that ended up in a fully medicalised all-the-interventions arrival for their baby that they didn’t want. And horrifically, even more hundreds wrote to share their stories of non-consenting, painful, and violating membrane sweeping when there was no reason for it, aside from the care provider’s decision that they had agency over their patient’s vagina and could do what they wanted when they wanted.
So what is it about membrane sweeping that is so cherished that challenging it generates death threats?
Buckle up. Here we go again!
©Hanna-Barbera
I’ve written about many topics over the years but nothing has ever generated as much discussion, opposition, and vitriol as challenging the cherished routine membrane sweep/stripping, aka stretch-and-sweep.
A few years ago, I wrote a post about how I’d like to see the routine, prior-to-40-weeks, without-medical-indication membrane sweep banned from obstetrical and midwifery practice. I talked about its risks and the fact that the clients I worked with called it a sexual assault when done without consent
The post went viral and I received hate messages and emails from around the world defending this procedure. In general, the sentiment was that I should most definitely be having sexual relations with myself, after which, I should be locked up and forever silenced. I also heard from hundreds of women whose births were ruined by days of painful, non-progressing contractions triggered by a membrane sweep that ended up in a fully medicalised all-the-interventions arrival for their baby that they didn’t want. And horrifically, even more hundreds wrote to share their stories of non-consenting, painful, and violating membrane sweeping when there was no reason for it, aside from the care provider’s decision that they had agency over their patient’s vagina and could do what they wanted when they wanted.
That particular post was prompted by a brief encounter with a new mother. Her baby was little and we got talking. She told me how she went to her usual prenatal visit at 36 weeks and the doctor said it was time for a vaginal check to see how things were coming along. She thought that was an ok idea and stripped accordingly, lay down on the examining table and put her feet in the stirrups. However, rather than a simple vaginal exam, she experienced excruciating pain that had her crawling up the table trying to escape that probing hand. The doctor removed her bloodied glove and when this woman asked why she was bleeding, the doctor responded, “That should get things going”. This mother had experienced a non-consenting, unplanned, and unknowing stretch-and-sweep to start labour before she or the baby were ready. She went home bleeding and cramping and within a few days went into labour and birthed a baby that was not ready to breathe. The baby spent 3 days in the NICU and she was devastated. Her birth was hijacked by a damnable routine from someone who should have known better or at least given a damn.
Yes, that was obstetrical violence. However, the routine of membrane sweeping for the mere reason that the client is at term is a deeply embedded ritual in obstetrics and mimicked by some midwives. I don’t think there is one other procedure that so callously turns a normally progressing pregnancy into a pathological event than this heinous routine.
So what is it about membrane sweeping that is so cherished that challenging it generates death threats?
Routines are habits that help organise our days
Let’s begin with some clarity on what I’m challenging.
First and foremost, I am not challenging the right for a pregnant person to choose a membrane sweep as a means of expediting labour. I fully support an individual’s right and autonomy to choose what is best for them.
Secondly, I am not challenging this as a tool for expediting labour when there is a medical indication.
I am challenging the ROUTINE of membrane sweeping that is done by some care providers as part of their normal and usual prenatal “package”, without any hint that there is a reason to expedite the birth of the baby due to an emerging medical condition.
At your cervix, ma’am
Let’s take a tour of the cervix. The cervix is a narrow passage that sits at the lower end of the uterus extending into the vagina. The cervix changes throughout the menstrual cycle and serves an important function in fertility. During ovulation, the cervix produces sperm-friendly mucus and becomes softer and more open to facilitate sperm reaching the ovum. When not ovulating, it produces sperm-unfriendly mucus and makes it more difficult for sperm to pass through to the uterus.
In pregnancy, the cervix fills with mucus, which creates a barrier to help prevent infection from passing through to the uterus. The cervix remains closed and rigid (like the tip of your nose) and is about 3-5 cm. long.
At term, in preparation for birth, the cervix will soften (like the inside of your cheek) due to the action of various hormones. The cervix is comprised of about 5-10% smooth muscle cells, which ensures it will stay closed and rigid throughout pregnancy. In preparation for labour, these muscle cells experience a programmed cellular death, which allows for the cervix to open (Leppert, 1995). The cervix will develop more oxytocin and prostaglandin receptors to help with the dilation process (Buckley, 2015). Prostaglandins, which are found abundantly in semen, ripens the cervix, digests the mucus plug, and promotes softening and shortening of the cervix.
Medical providers tend to give a great deal of attention to the cervix both prior to labour and in labour. It can provide some information that the medical folks find useful.
At term (around 40 weeks), the cervix can be felt to determine if it is ripening. Ripening means that the cervix is becoming softer, shorter, and is moving its position slightly forward. If so, it means that normal end-of-pregnancy hormones are doing their job. If not, it means that normal end-of-pregnancy hormones are doing their job, but they just haven’t gotten around to softening and shortening the cervix at the moment that a gloved hand is probing it.
This information is useful for planning an induction. A cervix that is shorter than 1.5 cm. is more predictive of spontaneous labour within the next 7-10 days than a longer cervix (Rao, Celik, Poggi, Poon, & Nicolaides, 2008). And a cervix that scores higher on the Bishop score is more predictive of an induction resulting in a vaginal birth rather than surgery (usually called “failure to progress”) (King, Pilliod, & Little, 2010). So that end-of pregnancy vaginal exam is about gathering information to plan your induction.
The other possibility for these routine (without medical indication) vaginal examinations in a healthy pregnancy is to develop submission and compliance in the client as she subjugates herself to the clinician by having her genitals penetrated by someone who is not her intimate partner.
Not too long ago, I was working with a postpartum client who was recovering from her birth experience. As a survivor of sexual assault she did not want anyone penetrating her genitals when she was labouring and giving birth and repeatedly told her midwife this. However, her midwife felt it was best for her to submit to vaginal exams in pregnancy to “get used to” them before she was in labour. Apparently, it never occurred to either of them that vaginal exams are optional and largely unnecessary for birthing a baby. In this case, the prenatal vaginal exams were for the purpose of building in submission and compliance so that the care providers could exercise agency over her body in labour.
Inductions: getting the baby out before it’s ready
An induction starts labour artificially before optimal hormonal physiology has prepared the baby and the mother for spontaneous birth. About 1 in 4 births begin by induction (BORN, 2013; Osterman & Martin, 2014). Although, there has been a slight decrease in inductions in recent years as fewer early-term inductions, meaning prior to 39 weeks, are performed. This has allowed more mothers to go into spontaneous labour without any additional adverse outcomes (Osterman & Martin, 2014). The cervix is one small part of the whole physiological process and since it can be reached easily by probing hands, it can provide a bit of information on whether an induction is likely to lead to a vaginal birth or is more likely to result in caesarean surgery.
There are lots of ways to artificially start labour before the mother or baby are ready. There are the so-called “natural” inductions:
Acupuncture and acupressure
Herbs and Homeopathy
Castor oil
Massage
Nipple stimulation
There are chemical inductions, which the literature calls “formal” inductions, as they require medical supervision:
Cervical ripening with prostaglandins
Intravenous synthetic oxytocin
And we have mechanical inductions, which also generally require medical supervision:
Artificial rupture of membranes aka “breaking the water”
Cervical ripening with a balloon catheter
Manual membrane sweeping/stripping, “stretch and sweep”
Ideally, an induction should only be suggested when the risks of staying pregnant outweigh the long and short-term risks of an induction. Depending on the method of induction those risks can include preterm birth, breathing problems in the baby, infection in the mother or baby, uterine hyper-stimulation, uterine rupture, fetal distress, breastfeeding failure, and rarely, death of either the mother or the baby.
Unfortunately, most inductions are done where the research affirms that the risks of an induction outweigh the risks of staying pregnant, including pre-labour rupture of membranes, gestational diabetes, suspected big baby, low fluid at term, isolated hypertension at term, twins, being “due”, or being “overdue” (Mozurkewich, Chilimigras, Koepke, Keeton, & King, 2009; Cohain, n.d.; Mandruzzato et al., 2010).
“membrane sweeping is a procedure meant to induce labour so that the client won’t be induced later”
Membrane sweeping: Fred Flintstone manipulating your physiology
Membrane sweeping involves the provider inserting their gloved hand into a mother’s vagina and manually stretching open the cervix and then running their finger around the opening of the cervix to separate the amniotic sack from the lower uterine segment. Caregivers will say it feels much like separating Velcro.
This procedure has the potential to trigger labour because it releases extra prostaglandins at the cervix. If the membrane sweep results in a shorter cervix, then it doesn’t make any difference in whether the mother is subsequently induced, but it does decrease the incidence of c-section. However, membrane sweeping is much more likely to result in cervical lengthening – which is predictive of NOT going into labour (Tan, Khine, Sabdin, Vallikkannu, & Sulaiman, 2011).
Prostaglandins are one of many important hormones that are needed for labour and birth. As pregnancy progresses and it’s getting time for the baby to be born, there are complex processes that prepare and protect the baby and are necessary for labour to commence. For example, the cervix and the uterus develop prostaglandin receptors so that necessary prostaglandins have a place to “land” or “connect” so that they can do their job. The uterus develops an abundance of oxytocin receptors so that this love hormone that is produced in the brain can connect with the uterus and cause contractions. The baby’s brain develops oxytocin receptors, which is neuro-protective for the journey ahead. There is an increase in estrogen, which activates the uterus for delivery. There are inflammatory processes within the uterus that help to mature the baby’s lungs to prepare for breathing on the outside. The baby’s brain develops increased epinephrine receptors to protect it from any gaps in oxygen during the birth. The mother’s brain develops endorphin receptors for natural pain relief. And there is an increase in prolactin to prepare the mother for breastfeeding and bonding. (Buckley, 2015)
When considering the finely-tuned and delicate interplay of complex and specific processes that brings the baby earth-side, a manual stretch-and-sweep at term without any medical indication is like getting Fred Flintstone to program an app that regulates the autonomic nervous system. It’s a crude, blunt instrument inserted into a complex system with the intention of bypassing evolutionarily necessary adaptive processes to cut the pregnancy short by a possible few days.
Let’s try to induce labour so we don’t have to induce labour
A Cochrane Review (Bouvain, Stan, & Irion, 2005) evaluated available studies comparing membrane sweeping to no sweeping. In general, this procedure can reduce the duration of pregnancy by up to three days. However, the authors noted that only small studies showed this reduction in pregnancy duration whereas larger studies didn’t, suggesting some bias. Because membrane sweeping doesn’t usually lead to immediate labour, it is not recommended when the need to get the baby out is urgent. Its primary use is to “prevent” a longer gestation and therefore an induction by more risky means.
A stretch-and-sweep is a procedure that is meant to induce labour so that you won’t be induced later. The Society of Obstetricians and Gynaecologists of Canada wrote in their 2013 Practice Guideline, which was reaffirmed in 2015, that “routine sweeping (stripping) of membranes promotes the onset of labour and that this simple technique decreases induction rates.”
Again: membrane sweeping is a procedure meant to induce labour so that the client won’t be induced later.
It assumes that the later induction is non-negotiable and the client’s best hope is that this early induction “saves” her from the risks of the later induction.
This is no different than all those “natural” inductions that are employed when trying to induce labour so the mother doesn’t have experience an induction – or the challenge of just declining the planned induction. It takes the approach that planned inductions are non-negotiable. Of course, mothers may chose a natural induction as a means of expediting the births of their babies for a number of reasons and I fully support their autonomy and choice to do so.
If there is a medical need to get the baby out to preserve its or its mothers life, then this dyad should be under medical supervision and receiving the best medical care possible. We need to critically evaluate the mentality that says, “let’s try to induce so we don’t have to induce”.
We’ve bought into a culture where non-evidence-based time limits and spurious reasons are given for booking inductions that don’t line up with the science. Rather than supporting mothers in exploring the science, doing a targeted risk/benefit analysis based on her particular situation, and supporting the mother in informed decision making, we line up the early inductions hoping to out-smart, out-wit, and out-play the medical providers who routinely induce based on outdated information or habit or hospital protocols that are based in their insurance risk-management strategy.
If this procedure is not recommended when there is an urgent need to get the baby out (Bouvain et al., 2005) and its primary purpose is to prevent a later induction where the indication is a pregnancy continuing beyond the cut-off date of the caregiver or institution (SOGC, 2013), then it has no medical indication.
What else did the Cochrane Review find?
There was a high level of bias in many of the studies, in part, because there could be no blinding. The clinicians knew they were performing the procedure and the clients knew they’d received it due to discomfort and pain
It was an out-patient procedure meaning there was no urgent reason for the induction
It did not generally lead to labour within 24 hours
No difference in oxytocin augmentation, use of epidural, instrumental delivery, caesarean delivery, meconium staining, admission to the NICU, or Apgar score less than seven at five minutes between sweeping and non-sweeping. This means it didn’t show any benefit
No difference in pre-labour rupture of membranes, maternal infection or neonatal infection. However, it’s worth noting that the non-sweeping participants were subject to routine obstetrical services that includes many vaginal exams that increase pre-labour rupture of membranes and infection (Maharaj, 2007; Zanella et al., 2010; Lenihan, 1984; Critchfield et al., 2013)
Significant pain in the mother during the procedure
Vaginal bleeding after the procedure
Painful contractions for the next 24 hours not leading to labour
What we have here is a routine that hurts the mother and has no significant benefit – aside from maybe possibly putting her into labour before another planned induction.
As the Cochrane Review discovered, the likely outcome of a membrane sweep is painful non-progressing contractions. This is often mis-interpreted as “labour” and the client is sent to the hospital for an induction anyway because she’s been “in labour” for 24-48 hours without progress. This is the epitome of a hijacked birth that turns a normal physiological process into a pathological one leading to the cascade of interventions, sometimes all the way up to an unwanted and unplanned caesarean for “failure to progress”. To convert the natural process into a pathological one is part of the classic definition of obstetrical violence (D'Gregorio, 2010).
They call it ‘birth rape’
For those who experienced this without their prior knowledge or consent, their comments overwhelmingly spoke of rape. This was especially pronounced in those with a history of prior rape. Studies confirm that those with a history of rape experience the routines of industrial birth differently than those without a history of sexual assault. For survivors, procedures that are uneventful for others can inadvertently put them “back in the rape” (Halvorsen, Nerum, Øian, & Sørlie, 2013).
Frankly, it’s unconscionable that any care provider would brazenly take the opportunity to manually manipulate a woman’s cervix, knowing it introduces risks and has the potential to hurt her, without the express knowledge and consent of the client following an informed choice discussion.
While membrane sweeping is intended to induce labour, it’s also used on labouring women to hurry things along. During labour, the cervix is being moved and thinned by the action of uterine muscles contracting and pulling the cervix up and around the baby’s head. The cervix is working hard and it’s tender. Many women will report that they screamed, cried ‘no’, tried to kick the provider’s hand away, or tried to crawl up the bed to get away from the invasive exam.
I remember one dark cold February night, years ago, when I was called to be with a family in labour. There was an ice storm and my trip there was dangerous and precarious. Eventually, my car slid into their street and managed to stop somewhere close to the driveway. I quietly entered the house to hear a mother in the throes of glorious, deep, active labour. I knew it wouldn’t be long before the baby arrived. I announced myself and tiptoed upstairs to see her on hands and knees with more blood than I would have expected on the towel beneath her. She said she invited her midwife to the birth and expected her to be there any minute. Soon enough, a beautiful baby boy gently emerged and landed safely into his daddy’s waiting hands. By the time the midwives arrived, the new family was tucked into bed enjoying a post-birth snack and cup of tea.
As the new family was bonding, I joined the midwives downstairs who were making notes in their client’s medical charts to make them some tea and offer a snack. I overheard one midwife say, “Oh yeah, when I was here earlier, she was about 6cm so I did a stretch-and-sweep”.
“Oh yeah.
Now I remember.
She was in active labour so I did an invasive and painful procedure to speed things up during a dark and dangerous ice storm.
Without her knowing I would do that.”
This is nothing but reckless cruelty. Yet this kind of cruelty permeates maternity services where women are routinely hurt for the sole purpose of interfering in their physiology and the safety of the birth process in order to get the baby out before they do even more risky and dangerous things.
And that is why I would like to see the ROUTINE, WITHOUT MEDICAL INDICATION membrane sweep removed from obstetrical and midwifery practice. It shouldn’t be the luck of the draw that a pregnant client gets one of the “good ones” who only induces a client when there is a medical need, with an informed choice discussion, and full consent.
To return to my original question: what is it about membrane sweeping that is so cherished that challenging it generates death threats?
It’s a deeply embedded ritual in a toxic medical culture that presumes to take authority over a pregnant woman’s sexual organs for the purpose of dominating the physiological process and then becoming a hero to the interrupted physiology and complications that ensue. It’s about power and control. And challenging this is a dangerous act of sedition. Those who do this to their clients like being the hero and clients who defend this need to believe they were saved from something – otherwise the truth is just too awful.
Make wise choices.
Much love,
Mother Billie
#endobstetricalnonsense #informedconsent #obstetricalviolence #membranesweeping #stretchandsweep #withoutconsent #birthrape #failuretoprogress
References
Better Outcomes Registry Network. (BORN). 2013. Provincial Overview of Perinatal Health in 2011–2012.
Boulvain, M., Stan, C. M., & Irion, O. (2005). Membrane sweeping for induction of labour. Cochrane Database of Systematic Reviews, (1).
Buckley, S. J. (2015). Hormonal physiology of childbearing: Evidence and implications for women, babies, and maternity care. Washington, DC: Childbirth Connection Programs, National Partnership for Women & Families.
Cohain, J. S. Reducing Inductions: Lack of Justification to Induce for “Postdates”.
Critchfield, A. S., Yao, G., Jaishankar, A., Friedlander, R. S., Lieleg, O., Doyle, P. S., ... & Ribbeck, K. (2013). Cervical mucus properties stratify risk for preterm birth. PloS one, 8(8), e69528.
D'Gregorio, R. P. (2010). Obstetric violence: a new legal term introduced in Venezuela.
Halvorsen, L., Nerum, H., Øian, P., & Sørlie, T. (2013). Giving birth with rape in one's past: a qualitative study. Birth, 40(3), 182-191.
King, V., Pilliod, R., & Little, A. (2010). Rapid review: Elective induction of labor. Portland: Center for Evidence-based Policy.
Lenihan, J. J. (1984). Relationship of antepartum pelvic examinations to premature rupture of the membranes. Obstetrics and gynecology, 63(1), 33-37.
Leppert, P. C. (1995). Anatomy and physiology of cervical ripening. Clinical obstetrics and gynecology, 38(2), 267-279.
Maharaj, D. (2007). Puerperal pyrexia: a review. Part II. Obstetrical & gynecological survey, 62(6), 400-406.
Mandruzzato, G., Alfirevic, Z., Chervenak, F., Gruenebaum, A., Heimstad, R., Heinonen, S., ... & Thilaganathan, B. (2010). Guidelines for the management of postterm pregnancy. Journal of perinatal medicine, 38(2), 111-119.
Mozurkewich, E., Chilimigras, J., Koepke, E., Keeton, K., & King, V. J. (2009). Indications for induction of labour: a best‐evidence review. BJOG: An International Journal of Obstetrics & Gynaecology, 116(5), 626-636.
Osterman, M. J., & Martin, J. A. (2014). Recent declines in induction of labor by gestational age.
Rao, A., Celik, E., Poggi, S., Poon, L., & Nicolaides, K. H. (2008). Cervical length and maternal factors in expectantly managed prolonged pregnancy: prediction of onset of labor and mode of delivery. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, 32(5), 646-65.
Rayburn, W. F., & Zhang, J. (2002). Rising rates of labor induction: present concerns and future strategies. Obstetrics & gynecology, 100(1), 164-167.
Society of Obstetricians and Gynaecologists of Canada. SOGC. 2013. Clinical Practice Guideline, No. 296, Indution of Labour.
Tan, P. C., Khine, P. P., Sabdin, N. H., Vallikkannu, N., & Sulaiman, S. (2011). Effect of membrane sweeping on cervical length by transvaginal ultrasonography and impact of cervical shortening on cesarean delivery. Journal of Ultrasound in Medicine, 30(2), 227-233.
Zanella, P., Bogana, G., Ciullo, R., Zambon, A., Serena, A., & Albertin, M. A. (2010). Chorioamnionitis in the delivery room. Minerva pediatrica, 62(3 Suppl 1), 151-153.
On the Art of Discussing Paradigm-Shifting Topics
Everyone has an intellectual/mental/emotional operating system – a personal paradigm that serves as a frame of reference containing basic assumptions and ways of thinking. This personal paradigm is the means by which we make sense of the world around us. It helps us to filter, understand, and categorise information and experiences. It helps us to know what is “true” and what isn’t; it guides our responses and our actions.
Humans are designed to be in connection with each other. We operate mostly unconsciously through hormones, synapses, and other magical pathways. Our primary operating system is our para-sympathetic nervous system – our “calm and connected” system. This part of our autonomic nervous system keeps our hearts beating, our lungs breathing, and our food digesting. The main hormone of this system is oxytocin – the hormone of love, trust, bonding, and connection. This is why isolation is so effective at crushing and changing people, and why friends and loved ones can heal and nurture new ideas.
Personal paradigms, once settled and serving us reasonably well are most likely to be changed by 2 things: Great Suffering or Great Love.
Everyone has an intellectual/mental/emotional operating system – a personal paradigm that serves as a frame of reference containing basic assumptions and ways of thinking. This personal paradigm is the means by which we make sense of the world around us. It helps us to filter, understand, and categorise information and experiences. It helps us to know what is “true” and what isn’t; it guides our responses and our actions.
Source: Paradigm Dramas in American Studies: A Cultural and Institutional History of the Movement. Gene Wise American Quarterly, Volume 31:3 (1979): 293-337.
For someone who was raised on the streets, relying on street-smarts and their wits, they may understand the world to be a hostile place with scarce resources and easily manipulated marks. This guides their responses and their actions. However, someone raised in a loving home with abundance and gentle guidance may understand the world to be an accommodating place where hard work and relationships lead to prosperity and contentment.
A personal paradigm develops over one’s lifetime and depends on many things,
One’s macro-culture – that’s the big stuff, like country of origin, current community, heritage, race, and cultural history
One’s micro-culture – that’s the smaller stuff, like family of origin, friends, current family members, or caregivers
Education – this includes the schools one attended, what was learnt, whether they felt successful in their education, and how the individual has continued to educate themselves, including interacting with mentors
Personal experiences – this is the stuff one has experienced in their lifetime and what it’s taught them about themselves, others, and the world around them
Media – the movies that are viewed, the stories read, the news that’s told, the images shown, the podcasts listened to, and the pages and the people followed
This is how we make sense of the world.
When someone is told that they are part of the privileged, they’re going to evaluate that against their personal paradigm, in particular, their personal experiences. They’ll be thinking of whether they were sent to school or educated. Whether they had enough food each day or a safe home to live in. Whether they were beat up or molested in childhood or how many important people in their life died. Or how many times they’ve been sexually assaulted. They may not feel particularly privileged.
Likewise, an individual whose life is filled with opportunity and meaningful relationships may not feel marginalised, despite sharing some characteristics or heritage with traditionally marginalised groups.
An individual with a background rife with adverse childhood experiences loses the perspective that theirs is a life of privilege when compared to those who are denied even more basic human rights due to race, ethnicity, gender, orientation, or heritage. Without connection with others against which to juxtapose their experiences, they are unlikely to understand the meaning of their privilege. Understanding comes through compassionate connection with those whose lives are different and with mentors who can lead the way.
Humans are designed to be in connection with each other. We operate mostly unconsciously through hormones, synapses, and other magical pathways. Our primary operating system is our para-sympathetic nervous system – our “calm and connected” system. This part of our autonomic nervous system keeps our hearts beating, our lungs breathing, and our food digesting. The main hormone of this system is oxytocin – the hormone of love, trust, bonding, and connection. This is why isolation is so effective at crushing and changing people, and why friends and loved ones can heal and nurture new ideas.
Personal paradigms, once settled and serving us reasonably well are most likely to be changed by 2 things: Great Suffering or Great Love.
Since I work in trauma, I see how Great Suffering rips out the core of an individual and changes their very identity, their very essence. And I see how Great Love can bring healing, restoration, a new way of viewing themselves and others, and a new way of interacting in the world.
When engaging in paradigm shifting conversations, such as privilege, racism, cultural appropriation, medical routines, consumerism, religion & faith, parenting, etc., there are a few things to consider:
What is your motive for engaging in the conversation?
Are you hoping to change the other person’s perspective? In this case, you’ll have to consider if you’ll employ Great Suffering or Great Love.
Will your conversation foster human connection?
Will everyone emerge from the conversation grateful for having been a part of it?
The key to engaging in a conversation that fosters human connection, and therefore, the opportunity to encourage paradigm-shifting changes, is empathy.
Empathy is the art of considering something from the other’s vantage, i.e. wearing their shoes (metaphorically) for a mile. It is connecting by establishing emotional resonance with the other person by placing oneself in their situation and looking through their eyes. Empathy is other-centred.
Sympathy is the art of considering something from our own vantage, by drawing upon our own experiences and feelings in order to connect through a shared or common experience or history. It is connection by looking inward in order to establish a common or shared experience. Sympathy is self-centred.
Empathy is the glue that holds us together as humans sharing life on this planet together. When I’m talking about paradigm-shifting conversations, I’m talking about communication between two or more reasonable people. This does not include narcissists or sociopaths. I’m also not talking about advocacy.
Lack of empathy is a defining characteristic of narcissists and sociopaths and they are generally impervious to connection based on achieving emotional resonance or to changing their perspective based on another’s suffering. It’s probably an exercise in futility to attempt to converse in paradigm-challenging topics.
Advocacy is a form of communication that elevates the voice(s) of those who are not being heard or are unable to speak for themselves. It seeks to ensure the voices of those who are disadvantaged, marginalised, oppressed, hurt, or excluded are represented. Their voices may be angry, frustrated, grieving, incensed, or frightened. Advocacy does not target an individual for reciprocal oppression, but rather brings awareness about systems and structures that permit individuals to oppress, hurt, exclude, and marginalise others. Advocacy opens eyes and brings people to the table to talk where empathy connects individuals. Connection, built on empathy, changes individuals who then leave oppressive systems and abandon marginalising behaviours to become agents of change and advocates.
Dominant cultures and dominant paradigms do not need to advocate for their own perspective. It is unnecessary to elevate their own voices or to engage in mockery, derision, denigration, or social isolation for the few that disagree with them.
unsplash.com
If we take today’s near hysteria regarding vaccines, how many families who no longer vaccinate their children, for whatever reason, including death or injury of a previously vaccinated child, moral objection to ingredients, scientific investigation, etc., have changed their minds as a result of having their children called “crotch fruit”, or being told they are too stupid to know vaccines save lives, that the lives of their children should be left to the professionals, or that they should be arrested and have their children taken from them? I’ll go out on a limb here and say “none”. Perhaps it’s a good example of how mockery, bullying, and denigration from a dominant group is more about bonding to their own kind than actually changing someone else’s perspective.
Personal paradigms are deeply entrenched operating systems. They don’t change because someone says we are wrong or someone says we are hurting others. Where advocacy opens eyes, empathy reaches deep into our limbic system where cherished beliefs are held. Empathy disarms fear; connection heals emotional wounds.
My paradigm-shifting changes happened because I was in connection with people who cared. They validated my concerns and shared their lives with me. I am changing my perspective on many things today because of deep connections that include mutual validation, concern, and love. I would no more want to hurt someone I care about by my thoughts or actions than I want to be hurt by another’s.
As privileged and marginalised peoples, we will only learn to connect in shared human experiences as members of this planet when we connect in love and empathy.
Paradigm-shifting conversations between two or more reasonable people begin with empathy for everyone’s learned experience, whether we’re talking about racism, privilege, cultural appropriation, marginalisation, consumerism, global warming, vaccinations, obstetrical violence, birth trauma, or veganism. Life has been tough for far too many people so far. Proceed with care.
Much love,
Mother Billie
unsplash.com
Birthing after Trauma – Seeing the Bigger Picture
It’s frustrating for care providers when their client comes armed with a 10-page birth plan, an army of doulas, and a mistrustful and hostile attitude. Care providers exist for the sole purpose of providing medical or midwifery services for pregnant, birthing, and postpartum clients and their goal is to help them emerge healthy and whole. Unfortunately, this creates friction before the relationship begins.
A mistrustful client has probably already had her trust broken by someone else long before they come armed with the minute details of how they need things to unfold. They may have already experienced abuse, neglect, sexual assault, victimisation, and trauma. Their trauma might have been the result of an abusive childhood, racial adversity, marginalisation, being the victim of a crime, or it might have been the result of a previous traumatic birth experience.
Published on Birth Trauma Ontario November 11, 2018
It Begins with a Mistrustful Client
Photo Martin Walls freeimages.com
It’s frustrating for care providers when their client comes armed with a 10-page birth plan, an army of doulas, and a mistrustful and hostile attitude. Care providers exist for the sole purpose of providing medical or midwifery services for pregnant, birthing, and postpartum clients and their goal is to help them emerge healthy and whole. Unfortunately, this creates friction before the relationship begins.
A mistrustful client has probably already had her trust broken by someone else long before they come armed with the minute details of how they need things to unfold. They may have already experienced abuse, neglect, sexual assault, victimisation, and trauma. Their trauma might have been the result of an abusive childhood, racial adversity, marginalisation, being the victim of a crime, or it might have been the result of a previous traumatic birth experience.
Birth Trauma Changes the Individual
Birth trauma doesn’t just happen. It’s not connected to an emergency or an unexpected outcome. These parents are not looking for someone to blame. Birth trauma is the result of clearly defined factors where the greatest indicator is a breakdown in the relationship between the care providers and the client (Harris & Ayers, 2012). The birthing mother felt disrespected, lied to, coerced, bullied, ignored, unsupported, and like she was just another cog in the wheel (Beck 2004; Reed, Reed, Sharman & Inglis, 2017). When this is partnered with pre-existing risk factors, this individual is at risk for developing postpartum post-traumatic stress disorder (Wu, Molteni, Ying, & Gomez-Pinilla, 2003; Faravelli, Giugni, Salvatori, & Ricca, 2004; Fromm, Heath, Vink, & Nimmo, 2004; Cortina &Kubiak, 2006; Eby & Eby, 2006; Sarandol et al., 2007; Lev-Wiesel, Chen, Daphna-Tekoah, & Hod, 2009; Roberts, Austin, Corliss, Vandermorris, & Koenen, 2010; Beck, Gable, Sakala, & Declercq, 2011; Cisternas et al., 2015; Matsumura et al., 2016; Du et al., 2016).
When parents have had a traumatic birth (about one third of all parents), they are much less likely to have another child, even if they wanted a larger family. In fact, they are twice as likely to not have another baby as someone who had a positive experience. If they choose to have another baby, the spacing between babies is twice as long as someone who had a positive experience. It takes them a much longer time to work up to doing it again (Gottvall & Waldenström, 2002).
Birthing after a traumatic experience is very different than preparing to birth a first child or another baby after a positive experience. These mothers are likely still dealing with the symptoms of trauma – flashbacks, sleep disturbances, terror, rage, difficulty forming new memories, hyperarousal always being on guard, and avoidance of triggers – including care providers and hospitals. These mothers are also more likely to be dealing with depression, anxiety, changes in their functional capacity, and suicidal thoughts than mothers without trauma. (DSM-5, 2013; Brady, Killeen, Brewerton, & Lucerini, 2000; Cook et al., 2004; Tavares et al., 2012).
When a Parent-of-Trauma Gets Pregnant Again
When a woman has had a traumatic birth and may still be suffering the effects of trauma, a new pregnancy can be a profoundly challenging time for her. She must now come face-to-face with the possibility that she will possibly endure the same horror in order to welcome this child into the world. Feelings of desperation, despair, fear, terror, and suicidal thoughts are not uncommon. Thoughts of running away and birthing alone in the woods are also common. This dread often interferes with bonding to her baby. (Beck & Watson, 2010)
The healthcare and birthing choices these parents make for subsequent births can be quite varied and diverse. Some might choose the same provider and location simply because it’s familiar and they know what’s coming. They know that they survived it the first time, and therefore can survive it again.
They might plan a caesarean section to gain the most control over the event. This way they can choose the surgeon, the day, and their support team. They won’t be facing the unknowns of whichever provider is on call.
If a mother chooses a vaginal birth, its very common for them to hire a doula as an advocate, to change providers, hospitals, plan a homebirth, or even birth in another city.
Unassisted Birth Choices
Freebirth, unassisted birth, or family birth, where there is no licensed medical attendant present, is a choice that is appearing more frequently in many developed countries (Holton & de Miranda, 2016). It’s a choice that is more common among parents who are birthing after trauma. Unassisted birth choices speak to the resistance that can be a response to the biomedical model of birth. Some families are finding that the obstetrical and midwifery model of risk-aversion and risk management removes their autonomy, and violates their culture, values, faith, or at times, their sexuality. If a mother has received disrespectful care, then they are more likely to avoid these services for subsequent pregnancies (UNPA, 2004). In an online survey of families that chose an unassisted birth, over half identified a previous negative hospital experience as the reason for their choice (O’Day, 2016). While there is no licensed medical attendant present, an unassisted birth may include the support of family members, doulas, traditional birth attendants, or other companions.
No matter what the mother-of-trauma chooses, she is disadvantaged because she can’t control for the behaviour of others in the medical system that don’t understand or respect her trauma or her perspective. Even the mother who chooses an unassisted birth may still be persecuted by hostile services if she transfers to the hospital for medical care (Vedam et al., 2017). Many a mother seeking medical support is “welcomed” by a harassing call to child protective services to investigate whether she is “conforming” to conventional medical services (Diaz-Tello, 2016). Online forums are filled with discussions on how to manage a possible trip to the hospital or doctor and how to prepare for a potentially harassing call to Childrens Aid Society (CAS), including sharing contact information for advocates and legal services. Indeed, misinformed providers are participating in this spiraling disconnect between clients and needed healthcare services.
Inappropriate Responses to Unconventional Choices
Providers will note that some of their clients decline the usual suite of obstetrical or midwifery services. For some clients, it’s an evidence-based decision. And for others, they are trying to avoid triggering their symptoms of trauma (Beck & Watson, 2010). Again, ill-equipped providers have been known to report these mothers to CAS, thinking that their health care choices are dangerous to the fetus. These are potentially well-meaning individuals, but have violated their professional ethics, as they cannot induce duress, bullying, or coercion to gain compliance (Health Care Consent Act, 1996). Further, the fetus has no citizenship and investigation by CAS regarding a fetus would be tantamount to harassment. However, this is one more obstacle that mothers-of-trauma often must navigate as they disentangle themselves from disrespectful care.
The consequence of these inappropriate actions from care providers is that mothers-of trauma will often decline further medical services for their babies once they are born, or to seek follow-up care or breastfeeding support (Finlayson & Downe, 2013; Moyer, Adongo, Aborigo, Hodgson, & Engmann, 2014). While pregnant, they may lie about their plans, their health, and other pertinent information, thereby missing an opportunity to form a collaborative relationship that could build lifetime wellness and resilience. They may choose to birth their babies without assistance and then tell their care provider that it just happened “too quickly”. This is ongoing evidence of the breakdown in the relationship between client and clinician.
Where Doulas Can Help
Doulas are the client’s and the clinician’s greatest ally as they generally develop the trust of the pregnant family and offer to serve as their advocate. Doulas can have a significant impact on the client’s outcome by reducing the need for surgery, assisted delivery, analgesia, and contributing to the reduction in low Apgars for the baby, and postpartum depression for the mother (Bohren, Hofmeyr, Sakala, Fukuzawa, & Cuthbert, 2017). Without the risk of reporting a non-compliant client, it is the doula that is privy to the client’s previous traumatic experience, the client’s coping strategies, and the wellbeing of the family. The doula has the opportunity to connect the client to resources in their community or to serve as a companion at medical visits. The rise of the doula to support families is indicative of a system that routinely denies birthing individuals informed choice, dignified care, and trauma-informed care (Dahlen, Jackson, & Stevens, 2011). Unfortunately, the burnout rate for doulas is very high due to vicarious trauma and institutional hostility (Naiman-Sessions, Henley, & Roth, 2017), meaning that experienced doulas are hard to find and it’s nearly impossible to foster their growth within the current medical paradigm.
© Billie Harrigan Consulting
Preparing to Birth After Trauma
When preparing to birth after trauma, the pregnant mother will often engage in a number of strategies that might seem excessive to someone who had a positive experience or to the provider who is not trauma-informed (Beck & Watson, 2010; Harrigan, 2017). These strategies can include:
Detailed, extensive, and lengthy birth plans
Hiring a doula
Doing extensive research into providers, locations, routines, and unassisted birth
Avoiding the usual suite of maternity services, such as ultrasound or scheduled prenatal visits
Doing birth art
Writing positive affirmations
Choosing complementary medicine to address health issues
Joining with other parents to learn more about birth, including how to have a breech baby, neonatal resuscitation, pre-eclampsia, etc.
Birth Plans – A Trauma Narrative in Disguise
Lengthy birth plans are generally the client’s attempt at communicating with their care team. It often represents their trauma narrative and is the care provider’s window into their client’s suffering that has brought them to this place. As a form of communication, however, it’s quite ineffective as far too many institutional cultures regard the birth plan as a joke where the longer the birth plan, the sooner she’s booked into the OR for a caesarean. Further, it has no impact on the care provider’s behaviour towards the client and may increase the client’s negative feelings about their birth (Berg, Lundgren, & Lindmark, 2003).
The client-of-trauma is again disadvantaged in trying to garner empathetic care in light of institutional hostility towards various modes of communication, including a birth plan, the use of a doula, self-advocacy, or the inclusion of other advocates. Attempts on the part of the client to change institutional culture are wholly ineffective if the entire facility isn’t addressing entrenched biases (Betrán et al., 2018).
It Begins with an Empathetic Trauma-Informed Care Provider
Photo credit: http://www.thefirsthelloproject.com
Birthing after trauma sometimes feels like a herculean feat for the mother where she is taken on a roller coaster of fear, despair, opposition, obstacles, institutional hostility, ill-equipped care providers, and unfortunately thoughts of suicide.
Yet, there is great hope. As more care providers become trauma-informed and institutions develop appropriate practices to support the client-of-trauma and develop a collaborative and respectful culture, the client can emerge with greater wellness, increased resilience, and growing trust. When a woman has a subsequent birth that fuels her post-traumatic growth, she credits the caring support of her care providers as a crucial element (Beck, 2010)
Nothing compares to the gift of a healing care provider.
Much love,
Mother Billie
References:
Beck, C. T. (2004). Birth trauma: in the eye of the beholder. Nursing Research, 53(1), 28-35.
Beck, C. T., & Watson, S. (2010). Subsequent childbirth after a previous traumatic birth. Nursing research, 59(4), 241-249.
Beck, C. T., Gable, R. K., Sakala, C., & Declercq, E. R. (2011). Posttraumatic stress disorder in new mothers: Results from a two‐stage US National Survey. Birth, 38(3), 216-227.
Berg, M., Lundgren, I., Lindmark G. (2003). Childbirth experience in women at risk: Is it improved by a birth plan? Journal of Perinatal Education. 12(2):1–15.
Betrán, A. P., Temmerman, M., Kingdon, C., Mohiddin, A., Opiyo, N., Torloni, M. R., ... & Downe, S. (2018). Interventions to reduce unnecessary caesarean sections in healthy women and babies. The Lancet, 392(10155), 1358-1368.
Bohren, M. A., Hofmeyr, G. J., Sakala, C., Fukuzawa, R. K., & Cuthbert, A. (2017). Continuous support for women during childbirth. The Cochrane Library.
Brady, K. T., Killeen, T. K., Brewerton, T., & Lucerini, S. (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. Journal of Clinical Psychiatry,61, 22-32.
Cisternas, P., Salazar, P., Serrano, F. G., Montecinos-Oliva, C., Arredondo, S. B., Varela-Nallar, L., ... & Inestrosa, N. C. (2015). Fructose consumption reduces hippocampal synaptic plasticity underlying cognitive performance. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease,1852(11), 2379-2390.
Cortina, L. M., & Kubiak, S. P. (2006). Gender and posttraumatic stress: sexual violence as an explanation for women's increased risk. Journal of abnormal psychology, 115(4), 753.
Cook, C. A. L., Flick, L. H., Homan, S. M., Campbell, C., McSweeney, M., & Gallagher, M. E. (2004). Posttraumatic stress disorder in pregnancy: prevalence, risk factors, and treatment. Obstetrics & Gynecology, 103(4), 710-717.
Coxon, K., Homer, C., Bisits, A., Sandall, J., & Bick, D. (2016). Reconceptualising risk in childbirth. Midwifery, 38, 1-5.
Dahlen, H. G., Jackson, M., & Stevens, J. (2011). Homebirth, freebirth and doulas: casualty and consequences of a broken maternity system. Women and Birth, 24(1), 47-50.
Diagnostic and Statistical Manual of Mental Disorders (DSM-5) American Psychiatric Assoc Pub; 5 edition(May 22 2013).
Diaz-Tello, F. (2016). Invisible wounds: obstetric violence in the United States. Reproductive Health Matters.
Du, J., Zhu, M., Bao, H., Li, B., Dong, Y., Xiao, C., ... & Vitiello, B. (2016). The role of nutrients in protecting mitochondrial function and neurotransmitter signaling: implications for the treatment of depression, PTSD, and suicidal behaviors. Critical reviews in food science and nutrition, 56(15), 2560-2578.
Eby, G. A., & Eby, K. L. (2006). Rapid recovery from major depression using magnesium treatment. Medical hypotheses, 67(2), 362-370.
Faravelli, C., Giugni, A., Salvatori, S., & Ricca, V. (2004). Psychopathology after rape. American Journal of Psychiatry, 161(8), 1483-1485.
Finlayson, K., & Downe, S. (2013). Why do women not use antenatal services in low-and middle-income countries? A meta-synthesis of qualitative studies. PLoS medicine, 10(1), e1001373.
Fromm, L., Heath, D. L., Vink, R., & Nimmo, A. J. (2004). Magnesium attenuates post-traumatic depression/anxiety following diffuse traumatic brain injury in rats. Journal of the American College of Nutrition, 23(5), 529S-533S.
Gottvall, K., & Waldenström, U. (2002). Does a traumatic birth experience have an impact on future reproduction?. BJOG: An International Journal of Obstetrics & Gynaecology,109(3), 254-260.
Harrigan, Billie. (2017). The Epic Failure of the Evidence-Based Movement. https://www.billieharrigan.com/blog/2017/1/16/the-epic-failure-of-the-evidence-based-movement.
Harris, R., & Ayers, S. (2012). What makes labour and birth traumatic? A survey of intrapartum ‘hotspots’. Psychology & Health, 27(10), 1166-1177.
Health Care Consent Act, 1996, S.O. 1996, c. 2, Sched. A
Holten, L., & de Miranda, E. (2016). Women׳s motivations for having unassisted childbirth or high-risk homebirth: An exploration of the literature on ‘birthing outside the system’. Midwifery.
Lev-Wiesel, R., Chen, R., Daphna-Tekoah, S., & Hod, M. (2009). Past traumatic events: are they a risk factor for high-risk pregnancy, delivery complications, and postpartum posttraumatic symptoms?. Journal of Women's Health, 18(1), 119-125.
Matsumura, K., Noguchi, H., Nishi, D., Hamazaki, K., Hamazaki, T., & Matsuoka, Y. J. (2016). Effects of omega-3 polyunsaturated fatty acids on psychophysiological symptoms of post-traumatic stress disorder in accident survivors: a randomized, double-blind, placebo-controlled trial. Journal of affective disorders.
Moyer, C. A., Adongo, P. B., Aborigo, R. A., Hodgson, A., & Engmann, C. M. (2014). ‘They treat you like you are not a human being’: maltreatment during labour and delivery in rural northern Ghana. Midwifery, 30(2), 262-268.
Naiman-Sessions, M., Henley, M. M., & Roth, L. M. (2017). Bearing the Burden of Care: Emotional Burnout Among Maternity Support Workers. In Health and Health Care Concerns Among Women and Racial and Ethnic Minorities (pp. 99-125). Emerald Publishing Limited.
O’Day, Katharine, L, "Outside the System": Motivations and Outcomes of Unassisted Childbirth. Transitions Midwifery Institute, Published online November 19, 2016.
Reed, R., Sharman, R., & Inglis, C. (2017). Women’s descriptions of childbirth trauma relating to care provider actions and interactions. BMC pregnancy and childbirth, 17(1), 21.
Roberts, A. L., Austin, S. B., Corliss, H. L., Vandermorris, A. K., & Koenen, K. C. (2010). Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. American Journal of Public Health, 100(12), 2433-2441.
Sarandol, A., Sarandol, E., Eker, S. S., Erdinc, S., Vatansever, E., & Kirli, S. (2007). Major depressive disorder is accompanied with oxidative stress: short‐term antidepressant treatment does not alter oxidative–antioxidative systems. Human Psychopharmacology: Clinical and Experimental, 22(2), 67-73.
Tavares, D., Quevedo, L., Jansen, K., Souza, L., Pinheiro, R., & Silva, R. (2012). Prevalence of suicide risk and comorbidities in postpartum women in Pelotas. Revista Brasileira de Psiquiatria, 34(3), 270-276.
United Nations Population Fund. (2004) in: UNFPA (Ed.) State of the World Population 2004. UNFPA, New York.
Vedam, S., Stoll, K., Rubashkin, N., Martin, K., Miller-Vedam, Z., Hayes-Klein, H., & Jolicoeur, G. (2017). The mothers on respect (MOR) index: measuring quality, safety, and human rights in childbirth. SSM-population health, 3, 201-210.
Wu, A., Molteni, R., Ying, Z., & Gomez-Pinilla, F. (2003). A saturated-fat diet aggravates the outcome of traumatic brain injury on hippocampal plasticity and cognitive function by reducing brain-derived neurotrophic factor. Neuroscience, 119(2), 365-375.
When not to induce – reason #408 – a placenta with calcium deposits
I received yet another phone call from someone who was trying to sort out the risks of staying pregnant versus the risks of being induced. From what the client could share, it was hard to know if the practitioner wasn’t fully informed on placental calcification at term, or wasn’t fully forthcoming about the non-clinical indications of that particular development in a healthy pregnancy.
To be sure, there are times when the benefits of an induction to rescue a compromised baby far outweigh the short and long-term risks of an induction.
Unfortunately, when trying to make an informed decision, clients often need to learn what their practitioners don’t know or won’t tell them.
“I’m 3 days overdue and my midwife says I need to be induced because my placenta is calcifying and that means it’s dying.”
I received yet another phone call from someone who was trying to sort out the risks of staying pregnant versus the risks of being induced. From what the client could share, it was hard to know if the practitioner wasn’t fully informed on placental calcification at term, or wasn’t fully forthcoming about the non-clinical indications of that particular development in a healthy pregnancy.
To be sure, there are times when the benefits of an induction to rescue a compromised baby far outweigh the short and long-term risks of an induction.
Unfortunately, when trying to make an informed decision, clients often need to learn what their practitioners don’t know or won’t tell them. So let’s take a little tour of the placenta.
© Billie Harrigan Consulting
To begin, the placenta is a fetal organ, meaning it is made from the same sperm and egg that makes the baby. As the baby grows and ages, so does the placenta. Both the baby and the placenta (which comes from the same genetic material) need to reach a certain level of maturity in order to be born healthy. The placenta does not suddenly expire when the pregnancy reaches an arbitrary number of weeks.
When the placenta is not well, the baby is usually not well. When the baby is well, then the placenta is usually well. Sometimes, there are variations in the placenta that are more common in babies at risk and they might also be present in a healthy baby. So not all variations mean something is wrong every time.
The placenta is a marvellous organ that has a maternal side that attaches to the wall of the mother’s uterus, and a fetal side where the umbilical cord arises to transport blood back and forth from the fetus to the placenta.
The umbilical cord usually has 2 arteries (going away from the baby’s heart towards the placenta) and one vein (returning back to the baby’s heart). So while blood that is full of oxygen is usually flowing through our arteries, in the case of the umbilical arteries, it’s going away from the baby to the placenta with waste and then the umbilical vein returns to the heart with oxygen and nutrients that are supplied by the placenta. The surrounding Wharton’s Jelly protects these important vessels inside the cord.
The mother’s blood and the baby’s blood don’t intermingle thanks to the wisdom of the placenta and the uterus working together. However, the baby gets all it’s nutrients from the mother’s blood stream and counts on mum to clean the waste the baby produces. Thanks to something called trophoblasts, which extend from the placenta into an area of the uterus where mum’s blood flows freely, oxygen and carbon dioxide and various nutrients and wastes are exchanged between mum and baby without baby’s blood and mum’s blood touching each other.
Khan Academy – meet the placenta
Due to the wonders of ultrasound, we’re now taking a look at things that were once hidden. And since we love to organise what we see and give things names, the placenta has been given names to indicate where it is in its development, as seen through ultrasounds:
Grade 0: less than 18 weeks gestation
Grade I: 18-29 weeks gestation
Grade II: 30-38 weeks gestation
Grade III: 39 weeks until birth
Each of these “grades” has specific features that help the technician to “date” the placenta.
One of the features of a Grade III placenta is that it often shows circular indentations that have calcium deposits (calcification). This is considered to be a natural part of the aging process in much the same way that our skin develops wrinkles as we age. And just as wrinkles in the skin of a person of any age doesn’t mean that this person is at risk of imminent death, neither does the appearance of calcification in a normal placenta at term mean that it’s about to expire (Harris & Alexander, 2000; Jamal et al., 2017; Nolan, 1998).
So where did this idea come from that calcification on a placenta meant it was dying?
This notion has come from the observation and study of preterm births of compromised fetuses. A compromised fetus that is born early often has a “grade III” placenta with significant calcification.
Image source: http://www.fetalultrasound.com/online/text/3-065.HTM
So while calcification of a placenta at term – around 39-42 weeks is part of the normal appearance of a full-term placenta and has no clinical significance in a healthy pregnancy, the appearance of significant calcification earlier in pregnancy is associated with risks to both the mother and baby. Just like we would be concerned about a very young person with wrinkles – it could be a sign of something significant happening.
Although, most every study has shown that calcification at term is normal and doesn’t mean anything in terms of negative outcomes for mum or baby, over the years, there has been conflicting evidence that early calcification was or wasn’t associated with poorer outcomes. That was because there were too many variables. In some studies, the mothers were smokers, which is associated with more calcification and more preterm births. In other studies, the mothers had hypertension, which can affect the health of the placenta and the baby. The studies were making comparisons on different ultrasound machines with interpretation by different technicians.
In a study of over 1000 pregnancies that controlled for these variables (Chen, Chen, & Lee, 2011), the participants agreed to frequent ultrasounds to monitor the development and progression of their baby’s placenta. The results indicated that when the placenta prematurely developed into a “grade III” with calcification prior to 32 weeks gestation, then,
The mother experienced increased
placental abruption
postpartum haemorrhage
transfer to the ICU
The baby experienced increased
preterm birth
low birth weight
low Apgar scores at 5 minutes (below 7)
neonatal death
However, if the placenta graduated to a “grade III” with calcification after 32 weeks gestation, then there were no increases in adverse outcomes. This was true whether the mother had other risk factors such as diabetes, hypertension, or smoking (Chen, Chen, & Lee, 2012).
Infarcts
Now let’s talk about those signs of “calcification” after the baby is born. Some placentas arrive with granular bumps across the maternal side and some parents are told that it’s a sign that the placenta was aging and starting to lose function. However, that’s not true for healthy full-term pregnancies.
Those granular bumps are not calcium deposits, but rather infarcts, deposits of fibrin, which are bits of scar tissue that have formed over dead cells through the process of infarction. Fibrin appears as small yellowish-white deposits that are the result of interference in the blood supply to the placenta.
Image source: http://wonderfullymadebelliesandbabies.blogspot.com/2012/11/variations-placentas-and-cords.html
Small placental infarctions (bumps of fibrin) are common in healthy full-term pregnancies and have no clinical significance. Only when there’s extensive infarction, meaning 10% or more of the placenta has died and been replaced by scar tissue is there an association with fetal growth restriction, fetal hypoxia, and fetal death, particularly if the infarctions occurred in the second and early third trimester (Mousa & Alfirevic1, 2000).
Infarcts can form at any point in the pregnancy and are associated with (Becroft, Thompson, & Mitchell, 2002; Naeye, 1977; Vinnars, Nasiell, Ghazi, Westgren, & Papadogiannakis, 2011):
maternal hyptertension
smoking
haemoglobin above 120, indicating poor blood volume expansion
maternal under-nutrition
So, in essence, when a mother is healthy and full term, calcification and infarcts are normal features of a healthy placenta – just like your healthy mother has some wrinkles and a few grey hairs.
This is one more bit of misinformation, mis-education, or pure nonsense that needlessly frightens healthy mothers into risky inductions.
Make wise choices, my friends.
Much love,
Mother Billie
References
Becroft, D. M. O., Thompson, J. M. D., & Mitchell, E. A. (2002). The epidemiology of placental infarction at term. Placenta, 23(4), 343-351.
Chen, K. H., Chen, L. R., & Lee, Y. H. (2011). Exploring the relationship between preterm placental calcification and adverse maternal and fetal outcome. Ultrasound in Obstetrics & Gynecology, 37(3), 328-334.
Chen, K. H., Chen, L. R., & Lee, Y. H. (2012). The role of preterm placental calcification in high-risk pregnancy as a predictor of poor uteroplacental blood flow and adverse pregnancy outcome. Ultrasound in medicine & biology, 38(6), 1011-1018.
Harris, R. D., & Alexander, R. D. (2000). Ultrasound of the placenta and umbilical cord. Ultrasonography in obstetrics and gynecology, 4, 597-625.
Jamal, A., Moshfeghi, M., Moshfeghi, S., Mohammadi, N., Zarean, E., & Jahangiri, N. (2017). Is preterm placental calcification related to adverse maternal and foetal outcome?. Journal of Obstetrics and Gynaecology, 37(5), 605-609.
Mousa, H. A., & Alfirevic1, Z. (2000). Do placental lesions reflect thrombophilia state in women with adverse pregnancy outcome?. Human Reproduction, 15(8), 1830-1833.
Naeye, R. L. (1977). Placental infarction leading to fetal or neonatal death. A prospective study. Obstetrics and gynecology, 50(5), 583-588.
Nolan, R. L. (1998). The placenta, membranes, umbilical cord, and amniotic fluid. A practical guide to ultrasound in obstetrics and gynecology, 438-439.
Vinnars, M. T., Nasiell, J., Ghazi, S. A. M., Westgren, M., & Papadogiannakis, N. (2011). The severity of clinical manifestations in preeclampsia correlates with the amount of placental infarction. Acta obstetricia et gynecologica Scandinavica, 90(1), 19-25.
Hocus Pocus - The ARRIVE study says inductions reduce caesareans
In an epic sleight of hand, the US obstetrical industry has managed to produce a study that affirms the “benefits” of universal elective induction of labour at 39 weeks. Headlines have trumpeted this remarkable accomplishment! Inducing labour early “prevents” c-sections!
The conclusion of the much anticipated ARRIVE study are presented in their abstract:
“IOL (induction of labour) in low-risk nulliparous women (first-time mothers) results in a lower frequency of CD (caesarean delivery) without a statistically significant change in the frequency of a composite of adverse perinatal outcomes.”
Obstetricians now have the much-desired go-ahead to routinely induce healthy first-time mothers prior to reaching 40 weeks under the guise that it will reduce c-sections with no additional negative outcomes to the mother or baby.
This is the same outrageous chicanery that brought us the ridiculously executed Term Breech Trial that changed obstetrical practices around the world. It was the excuse the industry was looking for to do what they already wanted to do: surgery.
In an epic sleight of hand, the US obstetrical industry has managed to produce a study that affirms the “benefits” of universal elective induction of labour at 39 weeks. Headlines have trumpeted this remarkable accomplishment! Inducing labour early “prevents” c-sections!
The conclusion of the much anticipated ARRIVE study (Grobman et al., 2018) are presented in their abstract:
“IOL (induction of labour) in low-risk nulliparous women (first-time mothers) results in a lower frequency of CD (caesarean delivery) without a statistically significant change in the frequency of a composite of adverse perinatal outcomes.”
Obstetricians now have the much-desired go-ahead to routinely induce healthy first-time mothers prior to reaching 40 weeks under the guise that it will reduce c-sections with no additional negative outcomes to the mother or baby.
This is the same outrageous chicanery that brought us the ridiculously executed Term Breech Trial that changed obstetrical practices around the world (Hannah et al., 2000). It was the excuse the industry was looking for to do what they already wanted to do: surgery (Hunter, 2013).
Obstetrics is a surgical speciality that also includes attending normal physiologic births. Years ago, the World Health Organisation sought to address disparities in health outcomes around the world in an effort to reduce maternal deaths in vulnerable places. They looked at countries with good outcomes and compared them to countries with poor outcomes. In wealthy nations where infrastructure was in place, food was easily accessible, and infection control measures were widely used, they tended to have a c-section rate around 5%. The WHO initially suggested that a c-section rate of 5-10% across the entire population could improve maternal-fetal outcomes. However, when the c-section rate rose above 15% across a population, the maternal death rate began to rise due to too much surgery.
There was naturally an outcry from the wealthy sector that was safely performing a lot of surgery and the WHO was roundly chastised for trying to prevent them from performing surgery on clients whom they believed would benefit from surgery. So the WHO said a c-section rate of 10-15% was “ideal” as it could potentially save lives, although they’ve subsequently stated that there is no benefit when the rate rises about 10% for a population (Betran, Torloni, et al, 2016).
Caesarean rates by country. (Betran, Ye, et al, 2016)
The problem wasn’t lack of surgery. The problem was that 99% of maternal deaths are in the developing world with half in sub-Sahara Africa and one-third in Southeast Asia where most fatal complications develop during pregnancy and are largely preventable or treatable. Half of these maternal deaths occur in fragile and humanitarian settings such as refugee displacement, natural disasters, and war (WHO, 2018).
Since the WHO’s mistake in encouraging an increase in surgery in impoverished, fragile, and humanitarian settings, the rest of the world’s obstetrics industry has spiraled out of control. Canada’s national c-section rate has risen to 28.2% in 2016-17 (CIHI, 2018) along with an increase in most every other country.
Data from around the world shows an average annual rate of increase in caesarean surgery of 4.4% from 1990 to 2014 (Betran, Ye, et al, 2016). Globally, in 2015 21.1% of all births occur through caesarean surgery, representing just over one in five mothers around the world (Boerma et al., 2018). This rate has risen from 12.1% of all births in 2000, representing a relative increase of 74.38% in just 15 years.
Regionally, caesarean rates are:
Latin America & Caribbean: 44.3% - an absolute increase of 19.4% and a relative increase of 77.91% (from 24.9% to 44.3%)
North America: 32.3% - an absolute increase of 10% and a relative increase of 44.84% (from 22.3% - 32.3%)
Oceania: 32.6% - an absolute increase of 14.1% and a relative increase of 76.22% (from 18.5% to 32.6%)
Europe: 27.3% - an absolute increase of 16.1% and a relative increase of 143.75% (from 11.2% to 27.3%)
Asia: 19.2% - an absolute increase of 15.1% and a relative increase of 343.18% (from 4.4% to 19.5%)
Africa: 7.3% - an absolute increase of 4.5% and a relative increase of 155.17% (from 2.9% to 7.4%)
Global increase in caesarean surgery 1990-2014. (Betran, Ye, et al, 2016)
What’s to blame for these shocking numbers? While it’s common to say it’s due to older, heavier, or more unhealthy mothers, the truth is that caesarean surgery has risen for every clientele group including young, slim, and healthy mothers.
The real increase in surgery comes from:
The management style of the hospital, where proactive management of patient flow and nursing resources results in more surgery and more postpartum haemorrhages (Plough et al., 2017)
Fear of litigation, particularly when malpractice premiums rise about $100,000 (Zwecker, Azoulay, & Abenhaim, 2011)
Financial incentives. Private facilities tend to perform more surgery as their clients have private insurance to pay for it (Dahlen et al., 2012). Even in the Canadian system, where compensation comes from a single payer through universal coverage, when the compensation for surgery is double that of a vaginal delivery, then there is a corresponding 5.6% increase in surgery when all else is equal (Allin, Baker, Isabelle, & Stabile, 2015)
Training, scheduling, and institutional culture drive the rates of surgery in individual institutions (Roth & Henley, 2012)
Both maternal request and maternal morbidity has been blamed for the dramatic increase in surgery, but neither has held up to scrutiny. The increase is physician induced (Roth & Henley, 2012).
Tomasz Kobosz freeimages.com
Now this same industry that has brought us shockingly high rates of surgery due to the nature of the industry says they have a “solution” for this epidemic: induce healthy mothers early.
The caesarean epidemic is due to the industry wanting to perform surgery. The unsupportable conclusions of the Term Breech Trial turned the industry upside-down in a heartbeat and most mothers with a breech-presenting baby are now faced with mandatory surgery. This industry is so invested in getting their way that some of their members have even resorted to using the courts to force clients into non-consenting procedures (Diaz-Tello, 2016).
The idea that inducing a mother early will reduce the incidence of caesarean surgery is akin to saying that if you give a child a pre-dinner snack then they are less likely to over-eat at dinner. Fulfilling the need to medically manage the client’s physiology satisfies the surgeon’s training, preferences, and institutional culture that guide the physician to perform surgery. This is nothing more than a physician placebo. And when this pre-dinner snack doesn’t satisfy any more, and the honeymoon phase of routine early induction wanes, then rates of surgery will rebound.
To begin, an induction is not benign. The risks associated with an induction depend on what is done to the patient. This could involve multiple vaginal exams (infection, sexual re-traumatisation), artificial rupture of membranes (cord prolapse, infection, foetal distress), continuous foetal monitoring (caesarean surgery), chemical cervical ripening (uterine hyperstimulation, uterine rupture, foetal distress, maternal death, foetal death, meconium), IV synthetic oxytocin (Pitocin/syntocinon) (uterine rupture, postpartum haemorrhage, breastfeeding failure, postpartum depression and anxiety, water intoxication leading to convulsions, coma or death, foetal distress, meconium, neonatal jaundice, neonatal brain damage, and neurological dysregulation in the child years later) (Gregory, Anthopolos, Osgood, Grotegut, & Miranda, 2013; Grotegut, Paglia, Johnson, Thames, & James, 2011; Gu et al., 2016; Kurth & Haussmann, 2011; Elkamil et al., 2011).
Inductions are generally more painful and first time mothers are more than 3x more likely to ask for an epidural during an induction (Selo-Ojeme et al., 2011). This leads to a longer labour and pushing stage, need for more synthetic oxytocin, problems passing urine, inability to move after the birth, fever, and more instrumental deliveries (Anim-Somuah, Smyth, Cyna, & Cuthbert, 2018).
Now let’s talk about the study itself.
A total of 3062 women were assigned to labour induction, and 3044 were assigned to expectant management (wait and see approach). Just like with the Term Breech Trial, there was quite a bit of crossover, meaning those who were assigned to the induction group had a spontaneous birth and those who were assigned to a wait-and-see approach were induced (about 5% from each group – 1 in 20 participants). However, the results were reported to the group they were assigned to.
The enrolment was designed to be too small to detect certain outcomes. Adverse outcomes such as maternal death, cardiac arrest, anaesthetic complications, thromboembolism, amniotic fluid embolism, major puerperal infection, or haemorrhage are fairly rare but are associated with both induction and surgery.
Without enough participants, it’s not possible to determine if there was an increase in adverse outcomes from inducing mothers.
Remember, this study took place in the US where they boast some of the worst maternal and neonatal outcomes in the developed world. How they practice obstetrics has much to do with this. Both the induction and the expectant management groups experienced high rates of interventions and the outcomes for the babies were consistent with that:
15% were not breathing at all or were breathing weakly 5 minutes after birth
12% were admitted to the NICU
5% had neonatal jaundice
1% needed breathing support for a day or more
0.7% experienced meconium aspiration syndrome
0.6% had hypoxic ischemic encephalopathy
0.3% suffered intracranial haemorrhage
0.3% had infections
0.2% had seizures
The results for the mothers were equally awful:
5% had severe postpartum haemorrhage of over 1500cc requiring a blood transfusion, blood products, or a hysterectomy
4% suffered a third or fourth degree perineal tear
2% had a postpartum infection
Benjamin Earwicker freeimages.com
With shockingly terrible results like this, the industry has the temerity to suggest that signing up for an elective induction to placate their nerves is a good idea because they’re less likely to perform surgery?
Frankly, it’s asinine nonsense from a group that needs a dramatic change in education and culture. We’ll see how long it takes for this insanity to move throughout the obstetrical world.
Make wise choices, my friends.
Much love,
Mother Billie
References
Allin, S., Baker, M., Isabelle, M., & Stabile, M. (2015). Physician Incentives and the Rise in C-sections: Evidence from Canada (No. w21022). National Bureau of Economic Research.
Anim-Somuah, M., Smyth, R. M., Cyna, A. M., & Cuthbert, A. (2018). Epidural versus non-epidural or no analgesia for pain management in labour. The Cochrane database of systematic reviews, 5, CD000331-CD000331.
Betrán, A. P., Torloni, M. R., Zhang, J. J., Gülmezoglu, A. M., WHO Working Group on Caesarean Section, Aleem, H. A., ... & Deneux‐Tharaux, C. (2016). WHO Statement on caesarean section rates. BJOG: An International Journal of Obstetrics & Gynaecology, 123(5), 667-670.
Betrán, A. P., Ye, J., Moller, A. B., Zhang, J., Gülmezoglu, A. M., & Torloni, M. R. (2016). The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PloS one, 11(2), e0148343.
Boerma, T., Ronsmans, C., Melesse, D., Barros, A., Barros, F., Juan, L., Moller, A., Say, L., Hosseinpoor, A., Mu, Y., Neto., D., Temmerman, M. (2018). Global epidemiology and use of and disparities in caesarean section. The Lancet. Volume 392, Issue 10155, P1341-1348, October 12, 2018.
CIHI. Canadian Institute for Health Information. (2018). Hospital Morbidity Database, 2016–2017.
Dahlen, H. G., Tracy, S., Tracy, M., Bisits, A., Brown, C., & Thornton, C. (2012). Rates of obstetric intervention among low-risk women giving birth in private and public hospitals in NSW: a population-based descriptive study. BMJ open, 2(5), e001723.
Diaz-Tello, F. (2016). Invisible wounds: obstetric violence in the United States. Reproductive Health Matters.
Elkamil, A. I., Andersen, G. L., Salvesen, K. Å., Skranes, J., Irgens, L. M., & Vik, T. (2011). Induction of labor and cerebral palsy: a population‐based study in Norway. Acta obstetricia et gynecologica Scandinavica, 90(1), 83-91.
Gommers, J. S., Diederen, M., Wilkinson, C., Turnbull, D., & Mol, B. W. (2017). Risk of maternal, fetal and neonatal complications associated with the use of the transcervical balloon catheter in induction of labour: A systematic review. European Journal of Obstetrics & Gynecology and Reproductive Biology, 218, 73-84.
Gregory, S. G., Anthopolos, R., Osgood, C. E., Grotegut, C. A., & Miranda, M. L. (2013). Association of autism with induced or augmented childbirth in North Carolina Birth Record (1990-1998) and Education Research (1997-2007) databases. JAMA pediatrics, 167(10), 959-966.
Grotegut, C. A., Paglia, M. J., Johnson, L. N., Thames, B., & James, A. H. (2011). Oxytocin exposure during labor among women with postpartum hemorrhage secondary to uterine atony. American journal of obstetrics and gynecology, 204(1), 56-e1.
Grobman, W. A., Rice, M. M., Reddy, U. M., Tita, A. T., Silver, R. M., Mallett, G., ... & Rouse, D. J. (2018). Labor induction versus expectant management in low-risk nulliparous women. New England Journal of Medicine, 379(6), 513-523.
Gu, V., Feeley, N., Gold, I., Hayton, B., Robins, S., Mackinnon, A., ... & Zelkowitz, P. (2016). Intrapartum synthetic oxytocin and its effects on maternal well‐being at 2 months postpartum. Birth, 43(1), 28-35.
Hannah, M. E., Hannah, W. J., Hewson, S. A., Hodnett, E. D., Saigal, S., Willan, A. R., & Collaborative, T. B. T. (2000). Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. The Lancet, 356(9239), 1375-1383.
Hunter, B. (2013). Implementing research evidence into practice: some reflections on the challenges. Evidence based midwifery, 11(3), 76-80.
Kurth, L., & Haussmann, R. (2011). Perinatal Pitocin as an early ADHD biomarker: neurodevelopmental risk?. Journal of attention disorders, 15(5), 423-431.
Linton, A., Peterson, M. R., & Williams, T. V. (2004). Effects of maternal characteristics on cesarean delivery rates among US Department of Defense healthcare beneficiaries, 1996–2002. Birth, 31(1), 3-11.
Plough, A. C., Galvin, G., Li, Z., Lipsitz, S. R., Alidina, S., Henrich, N. J., ... & McDonald, R. (2017). Relationship between labor and delivery unit management practices and maternal outcomes. Obstetrics & Gynecology, 130(2), 358-365.
Roth, L. M., & Henley, M. M. (2012). Unequal motherhood: racial-ethnic and socioeconomic disparities in cesarean sections in the United States. Social Problems, 59(2), 207-227.
Selo-Ojeme, D., Rogers, C., Mohanty, A., Zaidi, N., Villar, R., & Shangaris, P. (2011). Is induced labour in the nullipara associated with more maternal and perinatal morbidity?. Archives of gynecology and obstetrics, 284(2), 337-341.
Washington, S., Caughey, A. B., Cheng, Y. W., & Bryant, A. S. (2012). Racial and ethnic differences in indication for primary cesarean delivery at term: experience at one US Institution. Birth, 39(2), 128-134.
WHO, World Health Organization. (2018). Fact Sheet-Maternal Mortality.
Zwecker, P., Azoulay, L., & Abenhaim, H. A. (2011). Effect of fear of litigation on obstetric care: a nationwide analysis on obstetric practice. American journal of perinatology, 28(04), 277-284.
Me too
Recently, #metoo went viral as hundreds of thousands of women, and some men, said “me, too, I’ve been sexually harassed, assaulted or violated”. There were stories told for the first time. There were experiences re-told through a stronger voice. And in private forums, women told of rapes, childhood molestation, being drugged, and more. Some couldn’t post “me too” on their social media stories because they didn’t want their parents to know, believed they were partly to blame, or felt it was too exposing. One woman said she didn’t want the world to know she was “weak”. When asked, she said she wasn’t strong enough to fight off her attacker and she felt ashamed for it.
There were waves of trauma as some survivors found it too overwhelming to see the hundreds of #metoo’s across their news feeds and had to disconnect until it passed. It was not comforting to know they were not alone. It was horrifying.
And this isn’t just an issue of female looking or female identifying individuals being sexually violated. Men and boys are also sexually assaulted. Yet, from a cultural perspective, the response is different. Males are not told that “boys will be boys” or "girls will be girls" and they just normally like to grope and grab and hump and fondle males. Males are rarely depicted being sexually assaulted in music videos as a form of entertainment. They are not routinely asked what they were wearing, if they were out alone, if they went to a party, or if they were drinking. As a culture, we don’t victim blame males to the same extent that we victim blame females.
“You know sexual violence knows no race or color or gender or class. But the response to sexual violence does.” ~ Tarana Burke
Tarana Burke began the “me too” campaign in 2006 as a means of helping women who had been sexually assaulted not feel so alone. It was meant especially for girls and women of colour who had survived sexual violence to inspire empowerment through empathy. It was not only “to show the world how widespread and pervasive sexual violence is, but also to let other survivors know they are not alone.”
Recently, #metoo went viral as hundreds of thousands of women, and some men, said “me, too, I’ve been sexually harassed, assaulted or violated”. There were stories told for the first time. There were experiences re-told through a stronger voice. And in private forums, women told of rapes, childhood molestation, being drugged, and more. Some couldn’t post “me too” on their social media stories because they didn’t want their parents to know, believed they were partly to blame, or felt it was too exposing. One woman said she didn’t want the world to know she was “weak”. When asked, she said she wasn’t strong enough to fight off her attacker and she felt ashamed for it.
There were waves of trauma as some survivors found it too overwhelming to see the hundreds of #metoo’s across their news feeds and had to disconnect until it passed. It was not comforting to know they were not alone. It was horrifying.
And this isn’t just an issue of female looking or female identifying individuals being sexually violated. Men and boys are also sexually assaulted. Yet, from a cultural perspective, the response is different. Males are not told that “boys will be boys” or "girls will be girls" and they just normally like to grope and grab and hump and fondle males. Males are rarely depicted being sexually assaulted in music videos as a form of entertainment. They are not routinely asked what they were wearing, if they were out alone, if they went to a party, or if they were drinking. As a culture, we don’t victim blame males to the same extent that we victim blame females.
Unfortunately, as a group, female looking individuals beyond a certain age have almost universally been subjected to sexual objectification, harassment, violation or assault. And the problem is not that they are female looking, but that as a culture, we condone violence against them.
“Rape culture” is a term that describes a society that normalises sexual violence. Rape culture is perpetuated through the use of misogynistic language, the objectification of women’s bodies, and the glamorization of sexual violence, to the point where society disregards women’s rights and safety.
Sexual violence exists along a continuum that ranges from sexual remarks to sexual touching to rape. In a rape culture, both men and women assume that sexual violence is a fact of life. Rape culture includes jokes, TV, music, advertising, words, imagery and laws that make violence against women and sexual coercion seem so normal that people believe that it’s inevitable.
What does this do to women as they access health care services?
Some are keenly aware that they receive breast and pelvic examinations when there’s no logical reason for them. And some doctors will admit to getting some sexual gratification from performing these procedures. Yet, despite any ‘warning bells’ or intuition, women are told that any physical investigation by anyone with a medical licence is for their own good and is wholly benign and acceptable. Outside of medicine, we call this gaslighting.
Gaslighting is a form of manipulation where the individual is repeatedly told that their experience and their perceptions are wrong in order to cause the victim to doubt her or himself, and ultimately lose her or his own sense of perception, identity, and self-worth.
The annual pelvic exam (not the same thing as a pap test) is no longer recommended for asymptomatic women by the American College of Physicians, as a review of 70 year’s worth of studies shows it has no benefit in terms of detecting ovarian cancer, nor reducing deaths from ovarian cancer. It does, however, cause distress for more than one third of women who received these exams where survivors of sexual assault were more likely to find them painful, embarrassing and upsetting.
Yet despite the annual pelvic exam having no benefits for asymptomatic females and not being an evidence based procedure, ACOG remained firm that it was part of the “well-woman visit” that helped to establish “open communication”. It’s curious how having a provider’s hand inside a woman’s vagina, causing her embarrassment and discomfort, establishes open communication. It seems that she is expected to strip, lie down, spread her legs and take it. And this is her being a good girl, a good patient, and open to “communication” with her provider. Again, outside of medicine, we call this gaslighting.
For survivors of sexual abuse, the routine gynaecologic exam can provoke more intensely negative feelings including more trauma-like responses during the examination. This includes intrusive or unwanted thoughts, memories, body memories and feelings of detachment from their bodies. This is what is termed “re-experiencing”. Some survivors re-experience the sensations and memories of their sexual abuse during routine gynaecologic procedures (Robohm & Buttenheim, 1997).
Still, it’s normal for survivors to be told that the pelvic exam is nothing like their assault, and that they are out of their minds for even suggesting it. Comments on social media can take a quick turn to outrage that the provider isn’t a sexual abuser (even if he is - see below), thus derailing the conversation, which was to illuminate the survivor’s experience and then eventually to engage in a discussion about appropriate trauma informed clinical services. Again, it’s gaslighting to accuse the survivor who speaks of her personal experience of either saying the experience was not abusive when it was or of saying the clinician was the abuser when she is speaking of a memory or a flashback. The survivor is perfectly capable of distinguishing an assault from a memory. This manipulation is to ensure survivors are not to believe their sensations and perceptions and that no one else will believe them either. They are not to trust themselves but only what they are told.
Fortunately, most providers engage in sensitive and evidence based interactions with their clients. Given the high likelihood that most women have been the victim of sexual suggestion, objectification, discrimination, harassment, molestation, assault or rape, there are guidelines to help a clinician conduct a sensitive examination along with the assurance that the examination will stop when the client tells them to (Bates, Carroll, & Potter, 2011).
The doctor’s office is quite adaptive to trauma informed services for survivors, and in fact, might be the one place where the victim feels safe to reveal her history. The labour and delivery ward, however, can be highly problematic.
Modern institutional maternity services are designed to run with cost-and-time effective efficiency. Labour and delivery units have been modeled after Henry Ford’s manufacturing conveyor belt to ensure quick, efficient and uniform production and services (Perkins 2004). There are time limits (aka Friedman’s Curve) for each stage of labour where an intervention to speed things up helps to manage resources. Routines that have no benefit for the mother or baby (continuous electronic fetal monitoring, admission non-stress test) are applied as a means of lessening the potential for litigation while also introducing the potential for misdiagnosis and further interventions (Clarke, 2015).
The psychological aftermath of sexual assault, fear, anxiety, depression, fatigue, chronic pain, sleep or eating disturbances, self-harm, substance abuse and suicidal thoughts or attempts, have been termed Rape Trauma Syndrome (RTS). Those who suffer from Rape Trauma Syndrome have more serious symptoms than individuals who develop PTSD from other stressors. The closer the assault is to the legal definition of rape, forced and non-consenting sexual activity, the more intense the symptoms of RTS (Faravelli, Giugni, Salvatori, & Ricca, 2004).
Does a woman’s prior sexual abuse affect her experience of her provider’s services in birth? It can.
In interviewing mothers who had been raped and then gave birth, either vaginally or surgically, participants were given the opportunity to expand on their experience. As their narratives were analysed, the primary theme that emerged was that they experienced it as “being back in the rape” (Halvorsen, Nerum, Øian, & Sørlie, 2013).
During birth, their memories of their rape included:
Lying supine, forcibly restrained
Violent approach to the body/genitals
Painfully forced entry and vaginal penetration
Perpetrator takes over control of her body
Struggle, shouting, crying for help
Darkness, blood, semen, sweat, breath
Feels unclothed, despised
Helpless, degraded,
Gives up, lets it happen, feels ashamed, leaves her body, disappears
The triggers for these memories of their rape came from the routine conditions of their birth experience:
Being placed supine, physically restrained
Legs forced apart, placed in stirrups
Invasive procedures, not being listened to or seen
Invasive vaginal examinations
Unfamiliar hands touching body, being overruled
Sight/smell of blood, amniotic fluid, feces, sweat
Dimmed lighting/being unclothed
Bodily integrity not ensured
Being tied to bed or operating table, giving up
Birth attendants control body, room, time
In reflecting on this study, it’s not hard to understand why some women use the expression “birth rape”. Their births felt like a rape (Reed, Sharman, & Inglis, 2017).
For a mother who has been sexually assaulted, she may not experience the routines of birth, such as cervical exams, as benign. To her they may be sexually violating, particularly when the birth attendants don’t take the time to discuss the routines with her, ask her for her permission, wait for her to consent and then accept her refusal should she decline.
A critical issue in maternity services, as defined by the clients, is that maternal autonomy and consent are still nebulous concepts for many operators in the industry. In a survey of over 1500 doulas in the US and Canada (Roth et al., 2014),
71.2% had witnessed a care provider pull the dead baby card, i.e., tell a client that her baby might die if she didn’t agree to a proposed procedure
88.6% had witnessed a care provider engage in a procedure without giving the client a choice or time to consider the procedure
58.7% had witnessed a care provider engage in a procedure explicitly against the wishes of the client
The closer the assault is to the legal definition of rape, forced and non-consenting sexual activity, the more intense the symptoms of RTS (Faravelli et al., 2004). A woman who experiences her birth as forced and non-consenting sexual activity is at profound risk of negative physical, emotional, psychological and relational consequences.
#metoo happens in birth as well.
This isn’t to vilify individual providers within the maternity industry. It’s a cultural issue that is deep and complex. The hospital is a microcosm of the society in which it exists (Bowser & Hill, 2010). It is not set up to support clients who have already been subject to sexual violation. Just as much of society is not equipped to engage with their female members as equal partners.
In some hospitals, the client may choose to declare her past and set up an appointment with the hospital social worker to come up with a plan for respectful care that includes protecting her dignity, obtaining her consent and engaging in trauma informed care. Given how few individuals report sexual violations, it’s hard to have much faith in this approach. This depends on the victim declaring herself vulnerable in order to modify the behaviour of the staff. Is the client who does not expose her previous violations not afforded the same concessions of dignity, consent and trauma informed care?
And it’s not just hospitals where survivors are fighting to have their dignity and their rights respected. Home birth clients who have engaged a midwife can also experience the same difficulties in ensuring an appropriate trauma informed approach. A pregnant mother planning a home birth contacted Birth Trauma Ontario with this message: "I'm 37+3 and I met with my midwives this morning and they would like to terminate our relationship because they are concerned about the tone of my birth plan and feel that I am placing my baby in danger by declining routine pelvic exams during labour. What the f*ck do I do?" The mother was open to checks if there is a reason but didn't want regular exams every few hours. The midwife terminated their relationship shortly after her client sent this message.
When birthing clients register complaints about procedures done unnecessarily or without consent or after consent was removed, the typical response from the hospital or the regulatory body is that she didn’t understand what happened to her. She's told her provider was saving hers and her baby’s life. And she ought to be grateful. It’s one of the supremest forms of gaslighting and birthing women experience it all the time. Even in general society, when a mother talks about how difficult or traumatic her birth was or that her wishes were disregarded, the usual response is that she should be grateful, as the baby is all that matters. Somehow, we think babies can thrive with broken mothers if they just ignore their own needs enough.
Giving birth is pretty much the same, physiologically speaking, across most mammals, including humans. However, how we do birth is wholly cultural. In this culture of #metoo, women are expected to submit to routines and procedures that expose them, frighten them, penetrate them, and rob them of their dignity because it’s what women do to have a baby. Asking for a better experience is called selfish.
Rape culture affects all of us and it’s pervaded the delivery room where men sometimes still “joke” about a “husband stitch” to make her perineum nice and tight for the pleasure of the penis that will penetrate her after her recovery. Where women are still forced to birth on their backs in order to accommodate the skills limitations of the paid provider. Where strangers come and go. Where she receives routine cervical checks that are primarily for the benefit of the institution’s time and resource management. Where she is given no choice regarding the birth of her breech baby. Where she still hears providers pull the dead baby card in order to gain her compliance.
When Tarana Burke talks about how #metoo has gone viral, she is concerned whether those who helped to inspire women to disclose their stories of survival are prepared for what comes next.
There are many of us who are prepared. We understand that sexual violation writes on the fabric of who you are. We know that you sometimes want more time to choose your path – for birth and beyond without arbitrary time limits. We know that you don’t trust everyone, including yourself at times. We know that you have been manipulated and need to know that no one will use manipulation or coercion to gain your compliance. We know that you don’t want to be insulted by being told to stay off the internet. We understand that safety is more than a baby who is alive at the end of the process. It’s also about whether your spirit and your soul are alive as well. We know that you have requirements for your dignity and they may not be the same as your neighbour’s. We know that you don’t respect threats, lies or coercion. We know that if there’s going to be a power imbalance in the relationship, then you are the one with the power. We ask you for your truth as that’s more relevant that a practice guideline or a study.
As individuals are still reeling from the massive participation and revelation in the #metoo campaign, this is a good time to consider how we treat each other when it comes to personal boundaries and intimacy. Pregnancy, birth, and breastfeeding are deeply personal and intimate experiences. It’s time to take a good look at our rape culture for what it is and to begin to connect with birthing clients in a way that honours each one’s dignity, experiences and boundaries. We need to work together to ensure birthing families have real choices that respect their history, their values, their future, their hopes and their identity.
And for every person who said #metoo, there are hundreds and thousands more who didn’t say it but have experienced it nonetheless. Let’s be kind together and help each other heal. And let’s help each other to experience birth in a new culture of love and respect. Let’s learn the art of trauma informed care and learn to ask better questions and to offer options that really support each other. Together we are stronger.
Much love,
Mother Billie
References
Bates, C. K., Carroll, N., & Potter, J. (2011). The challenging pelvic examination. Journal of general internal medicine, 26(6), 651-657.
Bowser, D., & Hill, K. (2010). Exploring evidence for disrespect and abuse in facility-based childbirth. Boston: USAID-TRAction Project, Harvard School of Public Health
Clarke, E. (2015). Law and Ethics for Midwifery. Routledge.
Faravelli, C., Giugni, A., Salvatori, S., & Ricca, V. (2004). Psychopathology after rape. American Journal of Psychiatry, 161(8), 1483-1485.
Perkins, B. B. (2004). The medical delivery business: Health reform, childbirth, and the economic order. Rutgers University Press.
Halvorsen, L., Nerum, H., Øian, P., & Sørlie, T. (2013). Giving birth with rape in one's past: a qualitative study. Birth, 40(3), 182-191.
Reed, R., Sharman, R., & Inglis, C. (2017). Women’s descriptions of childbirth trauma relating to care provider actions and interactions. BMC pregnancy and childbirth, 17(1), 21.
Robohm, J. S., & Buttenheim, M. (1997). The gynecological care experience of adult survivors of childhood sexual abuse: a preliminary investigation. Women & health, 24(3), 59-75.
Roth LM, Heidbreder N, Henley MM, Marek M, Naiman-Sessions M, Torres J and Morton CH. (2014). Maternity Support Survey: A Report on the Cross-National Survey of Doulas, Childbirth Educators and Labor and Delivery Nurses in the United States and Canada.
The epic failure of the evidence-based movement
“All procedures offered to a mother should be researched by herself so she can make an informed decision.”
(posted on Facebook on a thread about routine interventions)“Make sure you hire a doula.”
(said by everyone)
Why are mothers being told to do their own research, find out more about their provider and their hospital, check out the alternatives, and make sure they can make an informed decision?
The pipe on my hot water tank sprung a leak and I called a plumber. Not once was I admonished to check into the possible things he might do to fix it and to decide if it was evidence based or if I should switch plumbers. He did a good job because if he didn’t, it would get around, and no one would hire him again.
And yet, mothers are urged to make sure they find out for themselves the risks of ultrasounds, what the science says about postdates, the risks of synthetic oxytocin (Pitocin/syntocinon), whether an epidural can cause problems, whether Friedman’s curve is actually useful for deciding on a “failure to progress” or if it’s a tool for the hospital to manage their time and resources, whether an induction for a big baby is evidence based, or if their provider supports a VBAC and what the risks are between VBAC and a repeat c-section. And if nothing else, hire a doula. And on it goes.
What’s behind this push for families to do their own research into the routines and interventions of birth? I think it’s been the epic failure of the evidence-based movement.
“All procedures offered to a mother should be researched by herself so she can make an informed decision.”
(posted on Facebook on a thread about routine interventions)
“Make sure you hire a doula.”
(said by everyone)
Why are mothers being told to do their own research, find out more about their provider and their hospital, check out the alternatives, and make sure they can make an informed decision?
The pipe on my hot water tank sprung a leak and I called a plumber. Not once was I admonished to check into the possible things he might do to fix it and to decide if it was evidence based or if I should switch plumbers. He did a good job because if he didn’t, it would get around, and no one would hire him again.
And yet, mothers are urged to make sure they find out for themselves the risks of ultrasounds, what the science says about postdates, the risks of synthetic oxytocin (Pitocin/syntocinon), whether an epidural can cause problems, whether Friedman’s curve is actually useful for deciding on a “failure to progress” or if it’s a tool for the hospital to manage their time and resources, whether an induction for a big baby is evidence based, or if their provider supports a VBAC and what the risks are between VBAC and a repeat c-section. And if nothing else, hire a doula. And on it goes.
What’s behind this push for families to do their own research into the routines and interventions of birth? I think it’s been the epic failure of the evidence-based movement.
Evidence-based medicine
The expression “evidence-based medicine” was introduced in 1991 in an ACP (American College of Physicians) Journal Club editorial and was quickly embraced. Medical clinical practice has been historically referred to as the “art of medicine” where expert opinion, experience and authoritarian judgement were the foundation for decision-making. Medicine held a strong distrust of biomedical research, scientific methodology and statistical analysis (Sur & Dahm, 2011). The problem was that medicine was lagging in accuracy and safety as other disciplines embraced these scientific tools. Obstetrics, in particular, was the medical discipline with the least sound practices, so much so, that Archie Cochrane awarded the discipline of obstetrics with the humiliating “wooden spoon” award in 1979. A decade later, A Guide to Effective Care in Pregnancy and Childbirth was published which seemed to usher in a new approach in obstetrics, and he agreed that it was time to withdraw his insult.
The most widely-accepted definition of evidence-based medicine is as follows:
“Evidence-based medicine [or care] is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research” (Sackett, 1996).
This sounds like the ideal where clients are both treated as individuals and are informed by the most current scientific information. However, this is not the experience of birthing mothers. Instead, mothers throughout the world, where obstetricians are the primary providers and hospitals are the primary birth location, are treated to what is largely a one-size-fits-all approach that resembles Henry Ford’s invention of the assembly line manufacturing plant (Perkins, 2004).
Policies that benefit the institution and the provider have replaced both common sense and holistic care. The widespread ban on VBACs (vaginal births after caesareans) in the US and the near universal unwillingness to support a vaginal breech birth speaks to the profit-before-sense kind of treatment that force women into increasingly unnecessary and risky surgeries without choice or individual care.
It’s also important to consider the limitations of “evidence-based” research. The randomised controlled trial (RCT) has been decided by committee to be the gold standard in research methodology. What this fails to recognise is that a birthing mother is an autonomous human who needs to be given a right to say what happens to her in birth. It’s unethical to randomly assign her to one arm of a research study without her ability to know what her choices are and to make an informed decision. Further, funding drives research. Only certain studies receive funding, which seldom extends beyond a brief time period. When interpreting research, one must consider the question being asked, the conditions under which it was asked, the parameters of the study, potential biases, limitations, and often, false conclusions (Ioannidis, 2005).
Increasing interventions
In the last several years, the rate of obstetrical interventions has increased dramatically without corresponding benefit. Increased interventions in low-risk mothers show an increase in neonatal morbidity (Dahlen et al., 2014). One would think that the evidence-based approach to maternity care would mean a reduced incidence of sick or hurt babies. Instead, money and profit has been a powerful motivator for increased use of interventions. It’s a well-documented fact that a mother in a private facility is more likely to have increased interventions and caesarean surgery than in a public facility. In other words, she’s more likely to have expensive services, like surgery, when she (or her insurance) has more money to offer (Dahlen et al., 2012).
Medical malpractice liability is another factor that influences the high rates of interventions and lessens the choices and autonomy provided to mothers. When the clinician or the facility is worried about being sued, they are more likely to use interventions and perform surgery (Morris, 2015).
Further, there is a direct relationship between a surgeon’s malpractice premiums and the rate of caesarean surgeries. In other words, the more that the provider pays for insurance, the more that caesarean surgeries are performed and the fewer VBACs that are supported (Yang, Mello, Subramanian, & Studdert, 2009).
The rates of interventions vary widely across countries, regions and even hospitals, including caesareans (Kozhimannil, Law, & Virnig, 2013), episiotomies (Graham, Carroli, Davies, & Medves, 2005), inductions (Tenore, 2003), and most every obstetric intervention. Certainly, differences in clientele would influence the rates of interventions in that a mother who is not well would have complications that require medical support. However, even that cannot explain the wide variation in obstetric interventions. The primary predictor of whether a low risk mother will receive a routine intervention is the kind of provider she has (Robinson, Norwitz, Cohen, & Lieberman, 2000).
Outdated practices
ACOG (American Congress of Obstetricians and Gynecologists) themselves admit that only about 25% of their obstetrical practice guidelines are based in good quality research. The rest is based in poor quality studies, opinion, and habit (Wright et al., 2011). The SOGC’s (Society of Obstetricians and Gynaecologists of Canada) practice guidelines are not much different in content. And frankly, no matter what the evidence says, most mothers get what’s offered and that’s often outdated protocols based on poor quality information, or habit.
We’ve known for 30 years that routine episiotomy, cutting the perineum to make a larger passage for the baby at birth, causes increased 3rd and 4th degree lacerations, increased fecal incontinence, and increased pain that can last years (Thorpe, Bowes Jr, Brame, & Cefalo, 1987; Borgatta, Piening, & Cohen, 1989; Klein et al., 1992; Signorello, Harlow, Chekos, & Repke, 2000; Hartmann et al., 2005). While the rate of episiotomies has been falling in most locations, according to the Listening to Mothers III Survey (US), 17% of women still had this procedure (Declercq, Sakala, Corry, Applebaum, & Herrlich, 2013).
“During the 40 minutes of pushing, the doctor turned to my mother and said, “I’m cutting her” and I yelled and begged for her NOT to cut me. But she ignored me and did it anyways. When she started to stitch me up, once again, I was screaming and begging for her to stop because it was extremely painful. I didn’t even know they were supposed to numb you first until recently.” (Carol, personal communication, 2016)
Back in the 1940’s it became routine to deny a mother any food in labor since she was going to be put under general anesthesia for her birth. The concern was that she would vomit under anesthesia and then aspirate (breathe) in the vomit and possibly die from the complications. Interestingly, it’s also been know for almost 30 years that fasting during labour doesn’t ensure gastric emptying (an empty stomach) and instead increases the acidity in her stomach, which is more problematic. And in fact, the likelihood of a mother dying from aspirating vomit during an emergency caesarean under general anesthesia is about 7 in 10,000,000 births (Sleutel & Golden, 1999). Further, forced fasting leads to a longer pushing stage (Rehamani, Khakbazan, Yavari, Granmayeh, & Yavari, 2012). No doubt that’s because labour burns up to 1000 calories per hour and the mother just gets tired from lack of nourishment.
The original recommendation in the 1940’s was based on worry and an attempt to exercise caution. There has been no corroborating evidence since then and any research has shown that eating and drinking brings comfort to mothers and reduces both pain and length of labour, so there is no reason to restrict the food they want (Singata, Tranmer, & Gyte, 2010). And yet, most mothers are not “allowed” to eat during labour when they birth in a hospital due to outdated and inflexible policies. Adding in a routine IV with glucose to replace real food just increases problems, as those newborns are more likely to have serious low blood sugar (Grylack, Chu, & Scanlon, 1984). So why aren’t most mothers eating in labour? Because hospitals don’t change outdated practices when it’s still working for them. Not providing food for labouring mothers saves money.
There are so many non-evidence based routines happening every day including:
Caesareans for failure to progress based on outdated time limits (Laughon, Branch, Beaver, & Zhang, 2012)
Routine induction at early term with a membrane stripping (Hill et al., 2008)
Routine induction for suspected fetal macrosomia (big baby) (Boulvain, Irion, Dowswell, & Thornton, 2016)
Induction for isolated (no other medical complications) oligohydramnios (low amniotic fluid) at term (close to your due date) (Manzanares et al., 2007)
Induction for isolated (no other complications) hypertension (high blood pressure) near term (Broekhuijsen et al., 2015)
Birthing on your back with your feet in the air or in stirrups, called a supine delivery (Terry, Westcott, O'Shea, & Kelly, 2006)
Staying in bed for labour (Bloom et al., 2008)
Continuous electronic fetal monitoring (Alfirevic, Devane, & Gyte, 2013)
Mandatory surgery for a breech presentation (Louwen, Daviss, Johnson, & Reitter, 2016)
Immediate cord clamping (Hutton, Reitsma, & Kaufman, 2007)
And on it goes.
“I remember telling my first doctor that I didn’t want or need rhogam at 27 weeks. I had researched it and because both my husband and I were negative blood type, it was impossible to have a positive baby. She told me I had no choice. It was mandatory.” (Joanne, personal communication, 2016)
How bad is it?
Consider that in the survey, Listening to Mothers III (US) (Declercq et al., 2013)
80% did not eat during labour
68% of mothers birthed on their backs
55% did not walk or move around during active labour
44% were induced for the reason that they were merely at term
16% were induced because the doctor was worried about a large baby
11% were induced because the doctor was worried about low fluid at term
10% had their public hair shaved for a vaginal birth
and when making a decision to have a repeat c-section rather than attempt a VBAC 63% said it was the doctor who made the decision
According to BORN Ontario (Niday Perinatal Database) 2005-2006 to 2009-2010 (BORN, 2011)
Inductions have risen from 21.8% in 2005-6 to 25.2% in 2009-10. A 15.6% increase in just 4 years cannot be explained by a massive shift in maternal-fetal wellbeing, but rather speaks to how quickly practitioners choose an intervention on a broad scale.
The rate of repeat c-sections increased 28.6% over that same time period
57.6% of elective repeat caesareans were performed before 39 weeks
18.3% of mothers had an episiotomy.
The caesarean section rate has increased every year across Canada from 18.7% in 1997 to 27.5% in 2014 where repeat surgery makes up more than half of this rise (CIHI, 2016). It seems that scheduled, profitable, daylight obstetrics is the driver behind this as there has been no new evidence of increased risk or harm to mothers or babies from VBAC births in the last several years.
What is stunning is that in spite of the evidence based movement, maternal mortality has risen in the US between 1990 and 2013 from 12 deaths per 100,000 to 28 per 100,000. Lack of consistent obstetrical practices has been identified as a major concern in this rising rate (Agrawal, 2015). And given the high rates of caesarean surgery, often due to policy or insurance premiums, it’s necessary to count the cost in lives lost due to excessive rates of surgery. Postpartum death is 3.6 times higher after a surgical birth than a vaginal birth (Deneux-Tharaux, Carmona, Bouvier-Colle, & Bréart, 2006).
In Canada, maternal mortality increased from 6 per 100,000 in 1990 to 11 per 100,000 in 2013. The question that begs to be answered is, where does the shocking increase in surgical birth fit into this decline in maternal safety?
Obstetric violence
In 2007, Venezuela became the first country to define obstetric violence through the Organic Law on the Right of Women to a Life Free of Violence.
In this law, obstetric violence is defined as:
“The appropriation of the body and reproductive processes of women by health personnel, which is expressed as dehumanized treatment, an abuse of medication, and to convert the natural processes into pathological ones, bringing with it loss of autonomy and the ability to decide freely about their bodies and sexuality, negatively impacting the quality of life of women.”
The following acts, executed by care providers, are considered obstetric violence:
1. Untimely and ineffective attention of obstetric emergencies;
2. Forcing the woman to give birth in a supine position, with legs raised, when the necessary means to perform a vertical delivery are available;
3. Impeding the early attachment of the child with his/her mother without a medical cause thus preventing the early attachment and blocking the possibility of holding, nursing or breast-feeding immediately after birth;
4. Altering the natural process of low-risk delivery by using acceleration techniques, without obtaining voluntary, expressed and informed consent of the woman;
5. Performing delivery via cesarean section, when natural childbirth is possible, without obtaining voluntary, expressed, and informed consent from the woman.
Obstetric violence is global and systemic (WHO, 2014). Having procedures performed that introduce risk without their knowledge or consent routinely violates mothers. Having her membranes broken in a healthy labour without indication, or having synthetic oxytocin unknowingly introduced into their IV, being forced onto her back for delivery, or having her genitals cut against her wishes are just the tip of the iceberg.
And yet, no one is holding the industry accountable. Obstetrical societies (ACOG, SOGC, et. al.) maintain a powerful lobbying presence with government to ensure that public policies and government spending are favourable to their industry. An absence of adequate oversight has allowed this industry to escalate their intrusion into healthy pregnancies to the point where 1 in 3 mothers say their births were traumatic and up to 1 in 10 mothers are grappling with postpartum PTSD as a result of their birthing experience (Beck, Gable, Sakala, & Declercq, 2011).
“I had a successful VBAC in a hospital. The next thing I know, an entire arm, up to her elbow, shoots into my vagina and uterus without any warning. I felt every inch of my placenta being ripped out of my uterus. I screamed at her to stop. Instead, the nurse pinned me down. PTSD robbed me of the next year of my life.” (Marie, personal communication, 2016)
The fact that the industry will not hold those providers and those institutions accountable for dangerous, outdated, and at times, abusive practices is simply stunning. Lateral violence (bullying, insults, coercion, sabotage, and even physical assault) within the industry keeps whistle blowers from speaking up, in particular nurses (Jackson et al., 2010). Nurses are especially vulnerable to lateral violence as the vast majority of nurses have been victims, most often from senior nurses (Christie, Jones, & PMHNPBC, 2014). This impacts their delivery of care to their patients and patient safety. In hospitals, nurses are the primary contact with the birthing family and the one in the best position to advocate for her patient and to report abusive or outdated care. Abusive behaviour within the nursing profession has contributed to preventing them from appropriately dealing with this failure on the part of the industry to give mothers the care they need and deserve.
The birth monopoly
Through clever marketing and expensive lobbying, obstetrics has gained a monopoly on birth. In most developed nations, hospitals have cornered the market on birth services and obstetricians, although more expensive and associated with more adverse outcomes in low risk populations, are the primary provider for most women. In places where midwifery is integrated into the health system, meaning they can facilitate a transfer to a hospital where her client will be accepted and the transfer is respectful and seamless, mothers have better outcomes at home with a midwife (Hutton, Reitsma, & Kaufman, 2009).
Physicians themselves are punished for providing true family centred care and risk losing hospital privileges for supporting a homebirth where the money doesn’t reach the institution. Like a dangerous cult, adherents (obstetricians) have even pursued a court order to force a mother to undergo mandatory caesarean surgery or called in child protective services to apprehend the children of mothers who disobeyed their dictates (Diaz-Tello, 2016).
“After 2 attempted homebirths that ended in caesareans, I was told that no midwife or doctor would support plans to have a homebirth VBAC. I could attempt a hospital VBAC but I would have to “fight” for it. To plan to attempt a vaginal birth at the same hospital, knowing that I would have to resist the system and medical staff every step of the way, was a recipe for failure and emotional distress.” (Lainie, personal communication 2016)
A few good folks
This is an industry-wide problem. However, there are truly wonderful individual providers who are doing their best to provide sensitive and individualised care with the best information they have. And they deserve credit, respect and thanks. Both doctors and midwives are routinely refused the opportunity to serve their clients in the manner they wish, perhaps through offering vaginal breech support, or not inducing according to policy when there is no medical indication. Yet these brave providers offer this care in the face of potentially sabotaging their opportunities for career advancement.
These providers are in high demand and are sometimes vilified by their colleagues whose excessive interventions bring more money into the industry coffers. They are shining diamonds in a deep mine and they make a difference in the lives of those fortunate enough to find them.
Individual nurses have taken the brunt of institutional hostility for advocating for their clients, for reporting unsafe practices, and for holding their colleagues to a higher standard. These are the professionals who deserve support and accolades.
Indeed, the evidence-based movement has been an epic failure that has left families reeling from their inability to influence their providers or the system that has set itself up to “save” her and her baby.
Families are paying the price
The true failure of the evidence-based movement has been the toll exacted on birthing families through lack of autonomy, lack of choice, excessive interventions, excessive surgery, birth trauma, and lives lost.
Due to the failure of the industry to deliver on their promise, we’ve entered the age where evidence based-medicine has become the responsibility of the consumer. Birthing families are urged to learn what their provider won’t learn or won’t practice.
When they are caught in a system run by dinosaurs, they are told that they didn’t do their research, they didn’t hire a doula, or they didn’t advocate for themselves. And the industry eats this up. They tell mothers to come in with a birth plan, all the while knowing that they see a birth plan as a direct route to more interventions (Grant, Sueda, & Kaneshiro, 2009).
A switch to a midwifery model of care with midwives providing the bulk of maternity services would mitigate some of these issues, as they’re more likely to use evidence-based care and to engage in informed consent and mother-centred care (Sandall, Soltani, Gates, Shennan, & Devane, 2016). However, a profitable industry with well-paid lobbyists won’t give up power and control easily. Obstetrics is currently a one-stop shop that provides a drive-through experience where everyone gets what’s on the menu.
You’ll note that when drawing attention to the need for mothers to do their own research or cautioning them to learn more about their provider before they consent to a routine, we hear total nonsense from industry members about not scaring mothers, not spreading misinformation, going with the flow, staying off the internet, and trusting the professionals. What they should be doing is apologising for aiding and abetting outdated protocols and industry-favourable policies that hurt mothers and babies and that it’s time to hold themselves accountable and rise to a higher standard.
Indeed, the evidence-based movement has been an epic failure that has left families reeling from their inability to influence their providers or the system that has set itself up to “save” her and her baby.
"I left the care of midwives when I caught them in lies and practices that went against informed choice. Despite what the medical system would have you believe, I had a wonderful and safe VBAC at home without a medical professional." (Chahna, personal communication, 2016)
The grassroots move to a new paradigm
Humans are resilient and they’ve always found a way to step away from systems that feel oppressive and to form communities that chart a path that honours their values, despite the risk of persecution. The rise of the DIY (do it yourself) birth movement, also called freebirth, unassisted, or family birth is a grassroots response that sees families taking care of each other outside of the obstetrical industry. There’s been a rise in unassisted homebirths in Sweden, Australia, Canada, the US, and Finland in response to the biomedical approach to birth and lack of autonomy for birthing mothers (Holten & de Miranda, 2016).
Of course, the obstetrical industry sees this as an exceptionally dangerous movement. Yet, their warnings may not match up with the experiences of the families themselves and may be more related to their position as a monopoly than the evidence of the safety of birth outside of their oversight.
In an anonymous online survey from December 2014 until September 2015, mothers who planned an unassisted birth responded (O’Day, 2016).
857 respondents from around the world
1449 babies born
1444 births (5 sets of twins)
1339 babies were born “unassisted”, meaning that there was no licensed attendant present although there might have been family, friends, doulas, or unregistered midwives.
The primary reason for choosing an unassisted birth was that they were led by their intuition (80.24%). The next most common reason was their dislike of hospitals (77.32%). They were also concerned for their newborn’s safety within a hospital setting (72.2%) and did not want to repeat a prior bad hospital experience (51.83%).
The results were interesting in the extraordinarily positive outcomes.
There were no maternal deaths
The neonatal death rate was 2.2 per 1000, which is comparable to the US rate of 2.97 per 1000
The caesarean rate was 1.24%
Of those who attempted a VBAC, 100% achieved it
Of those who had a VBAC, just over one quarter had had more than one previous caesarean
One third of the mothers had no prenatal services with a licensed provider, also called ‘prenatal care’ (this doesn’t account for community care and wellness measures)
Over 70% had no monitoring throughout labour and birth, i.e. no one listening to the baby’s heartbeat or routine vaginal exams
Just over 2% transported the newborn to a medical facility within the first week, mostly for breathing concerns
3.52% of the mothers transported for medical help after the baby was born primarily for postpartum haemorrhage
Certainly, this is a self-selecting group who responded to this survey. However, given that some of them were “high risk” in that they had had previous caesareans, had no prenatal care, and 5 were expecting twins, these results are seldom found within the medical obstetrical industry.
Once I decided not to continue prenatal care with the registered midwives, I was easily able to avoid trauma triggers and enjoy my pregnancy a lot more. The birth of my third baby was awesome! I was free to move around the whole house, I could eat or drink when I felt like it, I didn't have a single exam and I slept when I felt tired. I wasn't alone, but the people who were there didn't disturb me in any way. I never once wanted drugs for pain or to go to the hospital, it wasn't an option for me. My daughter had the best birth. No trauma, drama, drugs, strangers or tearing. Just a simple, healthy, happy family birth. (Samantha, personal communication, 2016)
© Billie Harrigan Consulting
As consumers have come to understand that the onus for evidence-based medicine has fallen on their shoulders, they’ve responded with outreach and connection. Online groups connect families to each other where they share research, studies, tips and encouragement. They share their medical history with one another and offer suggestions for self-care as well as recommendations for those providers and traditional birth attendants who support clients with holistic and scientifically sound care.
In-person groups are gathering to teach one another the physiology of birth, the mechanics of a vaginal breech birth, how to resolve a shoulder dystocia or a head entrapment, and to practice neonatal resuscitation skills.
Doulas are investing in advanced education and research skills to support their clients’ wishes for the evidence, access to their provider’s practice guidelines, and community connections and alternative care. Doulas are becoming specialists in supporting self-advocacy, research-based information, and helping clients connect to the services they need and want.
And as we learn more, we’re also discovering the importance of our microbiome and the epigenetic expression of our DNA where today’s one-size-fits-all comes across as pure buffoonery.
Taking back birth
We are at a crossroads in human history that will unfold over time. The “take back birth” movement is gaining momentum and this is being met with religious like zeal from the industry and its adherents in its opposition. They preach a different gospel where the modern medicalisation of birth and wholesale institutionalisation of birthing women has “saved” them. It’s a gospel that doesn’t hold up to scrutiny but nonetheless forms the lexicon of our culture (Tew, 2013).
So what can families do in light of the epic failure of evidence-based medicine?
Perhaps the answer lays in common sense.
Common sense dictates that if frequent prenatal visits and testing is upsetting, that the individual could just choose to bypass many of them. Science affirms that prenatal testing, no matter the results, increases maternal anxiety (Allison, Stafford, & Anumba, 2011). Prenatal anxiety is a risk factor for postpartum PTSD after a traumatic birth (Söderquist, Wijma, Thorbert, & Wijma, 2009). Maternal anxiety is also associated with poorer birth outcomes (Kumari & Joshi, 2014). And skipping those visits actually has no adverse outcome on the mum and baby and only affects the provider’s pocketbook (Walker, McCully, & Vest, 2001).
Common sense tells us that if a technology is useful for breaking up tissues such as cysts, scar tissue or kidney stones because it moves cells, then it might not be entirely safe for developing fetuses. Many parents are wary of ultrasound and their instincts tell them to bypass this routine. In fact, routine and frequent ultrasounds can contribute many problematic issues and has still not shown any benefit to mothers and babies, however it does increase inductions and caesareans (Cohain, 2011).
Common sense tells us that if we don’t want the gloved hand of someone we’re not in an intimate relationship with in our vaginas, we might want to decline as it may be more problematic than helpful (Lenihan, 1984).
Common sense suggests that if a hospital isn’t your cup of tea then birthing at home is a reasonable option (NICE, 2014).
Common sense and science are often aligned beautifully and generally support an individualistic approach to wellness, including birth, which takes into account a birthing mother’s physical, social, spiritual, and relational complexities. And as we learn more, we’re also discovering the importance of our microbiome and the epigenetic expression of our DNA where today’s one-size-fits-all comes across as pure buffoonery.
It’s going to be interesting to see how the medical industry responds to this growing grassroots movement. No doubt, lobbyists will pursue legislation to force mothers into the system for profit under the guise of “safety” which will drive families deeper underground. And should the numbers of families who choose to give birth outside the system actually have an impact on the profit margin of hospitals and obstetrical practices, then we’ll see a swift shift to “evidence-based” and “family-centred” care.
Until then, those good providers will do the best they can. Doulas will equip their clients with science and resources. And families will connect to support one another on this journey.
Evidence-based care has been an epic failure for parents but a mighty gold strike for the industry as they’ve cashed in on an illusion.
“I wish I knew then that I had the power to say NO. This is my body and we’re going to do this my way.” (Janice, personal communication, 2016)
References
Agrawal, P. (2015). Maternal mortality and morbidity in the United States of America. Bulletin of the World Health Organization, 93(3), 135-135.
Alfirevic, Z., Devane, D., & Gyte, G. M. (2013). Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. The Cochrane Library.
Allison, S. J., Stafford, J., & Anumba, D. O. (2011). The effect of stress and anxiety associated with maternal prenatal diagnosis on feto-maternal attachment. BMC women's health, 11(1), 1.
Beck, C. T., Gable, R. K., Sakala, C., & Declercq, E. R. (2011). Posttraumatic stress disorder in new mothers: Results from a two‐stage US National Survey. Birth, 38(3), 216-227.
Better Outcomes Registry & Network (BORN) Ontario. (2011). Perinatal Health Report 2009-2010. Greater Toronto Area (GTA) - LIHNs 5 to 9. Ottawa ON.
Bloom, S. L., McIntire, D. D., Kelly, M. A., Beimer, H. L., Burpo, R. H., Garcia, M. A., & Leveno, K. J. (1998). Lack of effect of walking on labor and delivery. New England Journal of Medicine, 339(2), 76-79.
Borgatta, L., Piening, S. L., & Cohen, W. R. (1989). Association of episiotomy and delivery position with deepperineal laceration during spontaneous delivery in nulliparous women. American journal of obstetrics and gynecology, 160(2), 294-297.
Boulvain, M., Irion, O., Dowswell, T., & Thornton, J. G. (2016). Induction of labour at or near term for suspected fetal macrosomia. The Cochrane Library.
Broekhuijsen, K., van Baaren, G. J., van Pampus, M. G., Ganzevoort, W., Sikkema, J. M., Woiski, M. D., ... & Rijnders, R. J. (2015). Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): an open-label, randomised controlled trial. The Lancet, 385(9986), 2492-2501.
Canadian Institute for Health Information, & Canadian Population Health Initiative. (2016). Improving the Health of Canadians. Summary Report [electronic Resource]. Canadian Institute for Health Information.
Christie, W., Jones, S., & PMHNPBC, R. (2014). Lateral violence in nursing and the theory of the nurse as wounded healer. OJIN: The Online Journal of Issues in Nursing, 19(1).
Cohain, J. S. (2011). Prenatal ultrasound does not improve perinatal outcomes. Midwifery today with international midwife, (102), 46-7.
Dahlen, H. G., Tracy, S., Tracy, M., Bisits, A., Brown, C., & Thornton, C. (2012). Rates of obstetric intervention among low-risk women giving birth in private and public hospitals in NSW: a population-based descriptive study. BMJ open, 2(5), e001723.
Dahlen, H. G., Tracy, S., Tracy, M., Bisits, A., Brown, C., & Thornton, C. (2014). Rates of obstetric intervention and associated perinatal mortality and morbidity among low-risk women giving birth in private and public hospitals in NSW (2000–2008): a linked data population-based cohort study. BMJ open, 4(5), e004551.
Declercq, E. R., Sakala, C., Corry, M. P., Applebaum, S., & Herrlich, A. (2013). Listening to MothersSM III.
Deneux-Tharaux, C., Carmona, E., Bouvier-Colle, M. H., & Bréart, G. (2006). Postpartum maternal mortality and caesarean delivery. Obstetrics & Gynecology, 108(3, Part 1), 541-548.
Diaz-Tello, F. (2016). Invisible wounds: obstetric violence in the United States. Reproductive Health Matters.
Graham, I. D., Carroli, G., Davies, C., & Medves, J. M. (2005). Episiotomy rates around the world: an update. Birth, 32(3), 219-223.
Grant, R., Sueda, A., & Kaneshiro, B. (2009). Expert opinion vs. patient perception of obstetrical outcomes in laboring women with birth plans. The Journal of reproductive medicine, 55(1-2), 31-35.
Grylack, L. J., Chu, S. S., & Scanlon, J. W. (1984). Use of intravenous fluids before caesarean section: effects on perinatal glucose, insulin, and sodium homeostasis. Obstetrics & Gynecology, 63(5), 654-658.
Hartmann, K., Viswanathan, M., Palmieri, R., Gartlehner, G., Thorp, J., & Lohr, K. N. (2005). Outcomes of routine episiotomy: a systematic review. Jama, 293(17), 2141-2148.
Hill, M. J., McWilliams, G. D., Garcia-Sur, D., Chen, B., Munroe, M., & Hoeldtke, N. J. (2008). The effect of membrane sweeping on prelabor rupture of membranes: a randomized controlled trial. Obstetrics & Gynecology, 111(6), 1313-1319.
Holten, L., & de Miranda, E. (2016). Women׳ s motivations for having unassisted childbirth or high-risk homebirth: An exploration of the literature on ‘birthing outside the system’. Midwifery.
Hutton, E. K., & Hassan, E. S. (2007). Late vs early clamping of the umbilical cord in full-term neonates: systematic review and meta-analysis of controlled trials. Jama, 297(11), 1241-1252.
Hutton, E. K., Reitsma, A. H., & Kaufman, K. (2009). Outcomes Associated with Planned Home and Planned Hospital Births in Low‐Risk Women Attended by Midwives in Ontario, Canada, 2003–2006: A Retrospective Cohort Study. Birth, 36(3), 180-189.
Ioannidis, J. P. (2005). Why most published research findings are false. PLoS Med, 2(8), e124.
Jackson, D., Peters, K., Andrew, S., Edenborough, M., Halcomb, E., Luck, L., ... & Wilkes, L. (2010). Trial and retribution: A qualitative study of whistleblowing and workplace relationships in nursing. Contemporary nurse, 36(1-2), 34-44.
Klein, M. C., Gauthier, R. J., Jorgensen, S. H., Robbins, J. M., Kaczorowski, J., Johnson, B., ... & Gelfand, M. M. (1992). Does episiotomy prevent perineal trauma and pelvic floor relaxation?. The Online journal of current clinical trials, 6019-words.
Kozhimannil, K. B., Law, M. R., & Virnig, B. A. (2013). Caesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Affairs, 32(3), 527-535.
Kumari, S., & Joshi, S. (2014). Birth outcomes following antenatal anxiety and depression.
Laughon, S. K., Branch, D. W., Beaver, J., & Zhang, J. (2012). Changes in labor patterns over 50 years. American journal of obstetrics and gynecology, 206(5), 419-e1.
Lenihan Jr, J. P. (1984). Relationship of antepartum pelvic examinations to premature rupture of the membranes. Obstetrics & Gynecology, 63(1), 33-37.
Lothian, J. (2006). Birth plans: the good, the bad, and the future. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 35(2), 295-303.
Louwen, F., Daviss, B. A., Johnson, K. C., & Reitter, A. (2016). Does breech delivery in an upright position instead of on the back improve outcomes and avoid caesareans?. International Journal of Gynecology & Obstetrics.
Manzanares, S., Carrillo, M. P., Gonzalez-Peran, E., Puertas, A., Montoya, F., Manzanares, S., ... & Montoya, F. (2007). Isolated oligohydramnios in term pregnancy as an indication for induction of labor. The Journal of Maternal-Fetal & Neonatal Medicine, 20(3), 221-224.
Morris, T. (2013). Cut it out: the C-section epidemic in America. NYU Press.
National Institute for Health and Care Excellence (NICE). (2014) Intrapartum care for healthy women and babies. Clinical guideline CG190.
O’Day, Katharine L. (2016). “Outside the System”: Motivations and Outcomes of Unassisted Childbirth. Published Online November 19, 2016, Sacred Transitions Midwifery Institute.
Perkins, B. B. (2004). The medical delivery business: Health reform, childbirth, and the economic order. Rutgers University Press.
Rahmani, R., Khakbazan, Z., Yavari, P., Granmayeh, M., & Yavari, L. (2012). Effect of oral carbohydrate intake on labor progress: randomized controlled trial. Iranian journal of public health, 41(11), 59.
Robinson, J. N., Norwitz, E. R., Cohen, A. P., & Lieberman, E. (2000). Predictors of episiotomy use at first spontaneous vaginal delivery. Obstetrics & gynecology, 96(2), 214-218.
Sackett, D. L. (1997, February). Evidence-based medicine. In Seminars in perinatology (Vol. 21, No. 1, pp. 3-5). WB Saunders.
Sandall, J., Soltani, H., Gates, S., Shennan, A., & Devane, D. (2016). Midwife‐led continuity models versus other models of care for childbearing women. Cochrane database of systematic reviews, (4).
Signorello, L. B., Harlow, B. L., Chekos, A. K., & Repke, J. T. (2000). Midline episiotomy and anal incontinence: retrospective cohort study. Bmj, 320(7227), 86-90.
Singata, M., Tranmer, J., & Gyte, G. M. (2010). Restricting oral fluid and food intake during labour. The Cochrane Library.
Sleutel, M., & Golden, S. S. (1999). Fasting in labor: relic or requirement. Journal of Obstetric, Gynecologic & Neonatal Nursing, 28(5), 507-512.
Söderquist, J., Wijma, B., Thorbert, G., & Wijma, K. (2009). Risk factors in pregnancy for post‐traumatic stress and depression after childbirth. BJOG: An International Journal of Obstetrics & Gynaecology, 116(5), 672-680.
Sur, R. L., & Dahm, P. (2011). History of evidence-based medicine. Indian Journal of Urology, 27(4), 487.
Tenore, J. L. (2003). Methods for cervical ripening and induction of labor. American family physician, 67(10), 2123-2128.
Terry, R. R., Westcott, J., O'Shea, L., & Kelly, F. (2006). Postpartum outcomes in supine delivery by physicians vs nonsupine delivery by midwives. The Journal of the American Osteopathic Association, 106(4), 199-202.
Tew, M. (2013). Safer childbirth?: a critical history of maternity care. Springer.
Thorp Jr, J. M., Bowes Jr, W. A., Brame, R. G., & Cefalo, R. (1987). Selected use of midline episiotomy: effect on perineal trauma. Obstetrics & Gynecology, 70(2), 260-262.
Walker, D. S., McCully, L., & Vest, V. (2001). Evidence‐based prenatal care visits: When less is more. Journal of Midwifery & Women’s Health, 46(3), 146-151.
World Health Organisation. (2014). The prevention and elimination of disrespect and abuse during facility-based childbirth: WHO statement.
Wright, J. D., Pawar, N., Gonzalez, J. S., Lewin, S. N., Burke, W. M., Simpson, L. L., ... & Herzog, T. J. (2011). Scientific evidence underlying the American College of Obstetricians and Gynecologists' practice bulletins. Obstetrics & Gynecology, 118(3), 505-512.
Yang, Y. T., Mello, M. M., Subramanian, S. V., & Studdert, D. M. (2009). Relationship between malpractice litigation pressure and rates of caesarean section and vaginal birth after caesarean section. Medical care, 47(2), 234.
The Textbook is Wrong
We were sitting across her kitchen table. A tissue was being nervously mangled in her trembling hands.
“I just can’t do it again,” she said. “Can you tell me about your daughter’s birth,” I asked her?
She explained that everyone told her it was a good birth. Her doctor said it was textbook perfect. Her mother was there and repeated her version of her granddaughter’s birth to everyone who would listen. It was natural. It was quick. It was the best day ever.
And as the story unfolded, tears welled up in my eyes, finally spilling down my own cheeks. It was an awful experience. And my heart broke into pieces again.
She described a birth where she was tortured with screamingly painful vaginal exams, weeping for them to stop, thrashing to escape the confines of the hospital bed where she was tethered to the monitoring machine for policy’s sake, begging to stand up, move, sway, anything to cope with her rapidly advancing labour. Her voice buried under a gentle shush so as not to scare the other mothers.
We were sitting across her kitchen table. A tissue was being nervously mangled in her trembling hands.
“I just can’t do it again,” she said. “Can you tell me about your daughter’s birth,” I asked her?
She explained that everyone told her it was a good birth. Her doctor said it was textbook perfect. Her mother was there and repeated her version of her granddaughter’s birth to everyone who would listen. It was natural. It was quick. It was the best day ever.
And as the story unfolded, tears welled up in my eyes, finally spilling down my own cheeks. It was an awful experience. And my heart broke into pieces again.
She described a birth where she was tortured with screamingly painful vaginal exams, weeping for them to stop, thrashing to escape the confines of the hospital bed where she was tethered to the monitoring machine for policy’s sake, begging to stand up, move, sway, anything to cope with her rapidly advancing labour. Her voice buried under a gentle shush so as not to scare the other mothers.
When the baby emerged, she was placed on her mother as the room cheered. Only, she felt nothing. Grateful that those hands wouldn’t enter her again, except in her dreams. The symptoms of PTSD followed her for the first year of her child’s life as she struggled to connect the version of her birth she’d been told and her personal experience of it.
And she just couldn’t do it again.
This is the story I hear over and over by mothers in all parts of the world. She’s told to be grateful for her healthy baby, to be grateful for the care she received, that her expectations were too high, that having a baby is hard and she had a low pain threshold, or that she was foolish for not taking the drugs offered her. She’s told anything except, “I’m sorry. It wasn’t meant to be that way.”
Research tells us that trauma is not particularly related to any emergencies or complications, but is dependent on how the mother experiences her birth. What can seem like a “textbook” birth to the clinician can be a devastating experience for the mother.
Birth is a hormonal process driven by our para-sympathetic nervous system, our “calm and connected” system. The primary driver of birth is oxytocin, which is the hormone of love, trust and bonding. Endorphins and prolactin ensure the experience is filled with pain-relief and joy. In today’s culture of fear, mothers are increasingly experiencing their births as traumatic as hospital policies serve the business end of cost-control, expediency, and insurance regulations. Doctors, nurses and midwives are sometimes constrained by policy in spite of the best interests of their clients.
Where birth is biologically programmed to be joyous, active, patient and primed for love and bonding, how we do birth in this culture is at odds with this biological imperative. The problem comes from what we call “textbook perfect”. The textbook is written from a medicalised perspective that is brand new in the biology of humans. Humans haven’t yet adapted to forced fasting, routine IVs, ultrasounds, continuous monitoring, hospital acquired infections, vaginal penetrations, forced on-her-back pushing, an inability to move and strangers between her legs.
When one third of mothers say their births were traumatic and one in ten struggle with PTSD, we know that birth is in crisis. And the textbook is wrong.
Of course, some births require medical assistance. Yet the question becomes, how can we protect a mother from trauma? And what happens when a pregnant mother says she can’t do that again?
In spite of the law that says a medical procedure cannot be performed on a non-consenting patient and that consent may be withdrawn at any point for any reason, the truth is that many things happen to a mother in labour in which she has no choice. In order to gain compliance, she may be told the baby might die. We call this ‘playing the dead baby card’ and it’s so common it’s becoming a laughing point.
There have been many a new textbooks written – from the mother’s perspective, from the baby’s perspective, from the vantage of good science, and yet mothers are still struggling. When a mother says she can’t do it again, it means we have to take a long hard look at what is happening today.
Strong and courageous leadership from medical associations including obstetricians, family physicians, nurses and midwives could lead the way in changing non-evidence based policies that serve the institution and insurance regulations but harm mothers and babies.
Mothers are increasingly learning the science of safe birth for themselves and are changing the conditions under which they give birth. Perhaps the quickest route to change is to spend our birthing dollars in those places that support the biology of birth and the law of informed consent and refusal.
It’s not selfish to want a great experience – it’s biology.