Me too
Recently, #metoo went viral as hundreds of thousands of women, and some men, said “me, too, I’ve been sexually harassed, assaulted or violated”. There were stories told for the first time. There were experiences re-told through a stronger voice. And in private forums, women told of rapes, childhood molestation, being drugged, and more. Some couldn’t post “me too” on their social media stories because they didn’t want their parents to know, believed they were partly to blame, or felt it was too exposing. One woman said she didn’t want the world to know she was “weak”. When asked, she said she wasn’t strong enough to fight off her attacker and she felt ashamed for it.
There were waves of trauma as some survivors found it too overwhelming to see the hundreds of #metoo’s across their news feeds and had to disconnect until it passed. It was not comforting to know they were not alone. It was horrifying.
And this isn’t just an issue of female looking or female identifying individuals being sexually violated. Men and boys are also sexually assaulted. Yet, from a cultural perspective, the response is different. Males are not told that “boys will be boys” or "girls will be girls" and they just normally like to grope and grab and hump and fondle males. Males are rarely depicted being sexually assaulted in music videos as a form of entertainment. They are not routinely asked what they were wearing, if they were out alone, if they went to a party, or if they were drinking. As a culture, we don’t victim blame males to the same extent that we victim blame females.
“You know sexual violence knows no race or color or gender or class. But the response to sexual violence does.” ~ Tarana Burke
Tarana Burke began the “me too” campaign in 2006 as a means of helping women who had been sexually assaulted not feel so alone. It was meant especially for girls and women of colour who had survived sexual violence to inspire empowerment through empathy. It was not only “to show the world how widespread and pervasive sexual violence is, but also to let other survivors know they are not alone.”
Recently, #metoo went viral as hundreds of thousands of women, and some men, said “me, too, I’ve been sexually harassed, assaulted or violated”. There were stories told for the first time. There were experiences re-told through a stronger voice. And in private forums, women told of rapes, childhood molestation, being drugged, and more. Some couldn’t post “me too” on their social media stories because they didn’t want their parents to know, believed they were partly to blame, or felt it was too exposing. One woman said she didn’t want the world to know she was “weak”. When asked, she said she wasn’t strong enough to fight off her attacker and she felt ashamed for it.
There were waves of trauma as some survivors found it too overwhelming to see the hundreds of #metoo’s across their news feeds and had to disconnect until it passed. It was not comforting to know they were not alone. It was horrifying.
And this isn’t just an issue of female looking or female identifying individuals being sexually violated. Men and boys are also sexually assaulted. Yet, from a cultural perspective, the response is different. Males are not told that “boys will be boys” or "girls will be girls" and they just normally like to grope and grab and hump and fondle males. Males are rarely depicted being sexually assaulted in music videos as a form of entertainment. They are not routinely asked what they were wearing, if they were out alone, if they went to a party, or if they were drinking. As a culture, we don’t victim blame males to the same extent that we victim blame females.
Unfortunately, as a group, female looking individuals beyond a certain age have almost universally been subjected to sexual objectification, harassment, violation or assault. And the problem is not that they are female looking, but that as a culture, we condone violence against them.
“Rape culture” is a term that describes a society that normalises sexual violence. Rape culture is perpetuated through the use of misogynistic language, the objectification of women’s bodies, and the glamorization of sexual violence, to the point where society disregards women’s rights and safety.
Sexual violence exists along a continuum that ranges from sexual remarks to sexual touching to rape. In a rape culture, both men and women assume that sexual violence is a fact of life. Rape culture includes jokes, TV, music, advertising, words, imagery and laws that make violence against women and sexual coercion seem so normal that people believe that it’s inevitable.
What does this do to women as they access health care services?
Some are keenly aware that they receive breast and pelvic examinations when there’s no logical reason for them. And some doctors will admit to getting some sexual gratification from performing these procedures. Yet, despite any ‘warning bells’ or intuition, women are told that any physical investigation by anyone with a medical licence is for their own good and is wholly benign and acceptable. Outside of medicine, we call this gaslighting.
Gaslighting is a form of manipulation where the individual is repeatedly told that their experience and their perceptions are wrong in order to cause the victim to doubt her or himself, and ultimately lose her or his own sense of perception, identity, and self-worth.
The annual pelvic exam (not the same thing as a pap test) is no longer recommended for asymptomatic women by the American College of Physicians, as a review of 70 year’s worth of studies shows it has no benefit in terms of detecting ovarian cancer, nor reducing deaths from ovarian cancer. It does, however, cause distress for more than one third of women who received these exams where survivors of sexual assault were more likely to find them painful, embarrassing and upsetting.
Yet despite the annual pelvic exam having no benefits for asymptomatic females and not being an evidence based procedure, ACOG remained firm that it was part of the “well-woman visit” that helped to establish “open communication”. It’s curious how having a provider’s hand inside a woman’s vagina, causing her embarrassment and discomfort, establishes open communication. It seems that she is expected to strip, lie down, spread her legs and take it. And this is her being a good girl, a good patient, and open to “communication” with her provider. Again, outside of medicine, we call this gaslighting.
For survivors of sexual abuse, the routine gynaecologic exam can provoke more intensely negative feelings including more trauma-like responses during the examination. This includes intrusive or unwanted thoughts, memories, body memories and feelings of detachment from their bodies. This is what is termed “re-experiencing”. Some survivors re-experience the sensations and memories of their sexual abuse during routine gynaecologic procedures (Robohm & Buttenheim, 1997).
Still, it’s normal for survivors to be told that the pelvic exam is nothing like their assault, and that they are out of their minds for even suggesting it. Comments on social media can take a quick turn to outrage that the provider isn’t a sexual abuser (even if he is - see below), thus derailing the conversation, which was to illuminate the survivor’s experience and then eventually to engage in a discussion about appropriate trauma informed clinical services. Again, it’s gaslighting to accuse the survivor who speaks of her personal experience of either saying the experience was not abusive when it was or of saying the clinician was the abuser when she is speaking of a memory or a flashback. The survivor is perfectly capable of distinguishing an assault from a memory. This manipulation is to ensure survivors are not to believe their sensations and perceptions and that no one else will believe them either. They are not to trust themselves but only what they are told.
Fortunately, most providers engage in sensitive and evidence based interactions with their clients. Given the high likelihood that most women have been the victim of sexual suggestion, objectification, discrimination, harassment, molestation, assault or rape, there are guidelines to help a clinician conduct a sensitive examination along with the assurance that the examination will stop when the client tells them to (Bates, Carroll, & Potter, 2011).
The doctor’s office is quite adaptive to trauma informed services for survivors, and in fact, might be the one place where the victim feels safe to reveal her history. The labour and delivery ward, however, can be highly problematic.
Modern institutional maternity services are designed to run with cost-and-time effective efficiency. Labour and delivery units have been modeled after Henry Ford’s manufacturing conveyor belt to ensure quick, efficient and uniform production and services (Perkins 2004). There are time limits (aka Friedman’s Curve) for each stage of labour where an intervention to speed things up helps to manage resources. Routines that have no benefit for the mother or baby (continuous electronic fetal monitoring, admission non-stress test) are applied as a means of lessening the potential for litigation while also introducing the potential for misdiagnosis and further interventions (Clarke, 2015).
The psychological aftermath of sexual assault, fear, anxiety, depression, fatigue, chronic pain, sleep or eating disturbances, self-harm, substance abuse and suicidal thoughts or attempts, have been termed Rape Trauma Syndrome (RTS). Those who suffer from Rape Trauma Syndrome have more serious symptoms than individuals who develop PTSD from other stressors. The closer the assault is to the legal definition of rape, forced and non-consenting sexual activity, the more intense the symptoms of RTS (Faravelli, Giugni, Salvatori, & Ricca, 2004).
Does a woman’s prior sexual abuse affect her experience of her provider’s services in birth? It can.
In interviewing mothers who had been raped and then gave birth, either vaginally or surgically, participants were given the opportunity to expand on their experience. As their narratives were analysed, the primary theme that emerged was that they experienced it as “being back in the rape” (Halvorsen, Nerum, Øian, & Sørlie, 2013).
During birth, their memories of their rape included:
Lying supine, forcibly restrained
Violent approach to the body/genitals
Painfully forced entry and vaginal penetration
Perpetrator takes over control of her body
Struggle, shouting, crying for help
Darkness, blood, semen, sweat, breath
Feels unclothed, despised
Helpless, degraded,
Gives up, lets it happen, feels ashamed, leaves her body, disappears
The triggers for these memories of their rape came from the routine conditions of their birth experience:
Being placed supine, physically restrained
Legs forced apart, placed in stirrups
Invasive procedures, not being listened to or seen
Invasive vaginal examinations
Unfamiliar hands touching body, being overruled
Sight/smell of blood, amniotic fluid, feces, sweat
Dimmed lighting/being unclothed
Bodily integrity not ensured
Being tied to bed or operating table, giving up
Birth attendants control body, room, time
In reflecting on this study, it’s not hard to understand why some women use the expression “birth rape”. Their births felt like a rape (Reed, Sharman, & Inglis, 2017).
For a mother who has been sexually assaulted, she may not experience the routines of birth, such as cervical exams, as benign. To her they may be sexually violating, particularly when the birth attendants don’t take the time to discuss the routines with her, ask her for her permission, wait for her to consent and then accept her refusal should she decline.
A critical issue in maternity services, as defined by the clients, is that maternal autonomy and consent are still nebulous concepts for many operators in the industry. In a survey of over 1500 doulas in the US and Canada (Roth et al., 2014),
71.2% had witnessed a care provider pull the dead baby card, i.e., tell a client that her baby might die if she didn’t agree to a proposed procedure
88.6% had witnessed a care provider engage in a procedure without giving the client a choice or time to consider the procedure
58.7% had witnessed a care provider engage in a procedure explicitly against the wishes of the client
The closer the assault is to the legal definition of rape, forced and non-consenting sexual activity, the more intense the symptoms of RTS (Faravelli et al., 2004). A woman who experiences her birth as forced and non-consenting sexual activity is at profound risk of negative physical, emotional, psychological and relational consequences.
#metoo happens in birth as well.
This isn’t to vilify individual providers within the maternity industry. It’s a cultural issue that is deep and complex. The hospital is a microcosm of the society in which it exists (Bowser & Hill, 2010). It is not set up to support clients who have already been subject to sexual violation. Just as much of society is not equipped to engage with their female members as equal partners.
In some hospitals, the client may choose to declare her past and set up an appointment with the hospital social worker to come up with a plan for respectful care that includes protecting her dignity, obtaining her consent and engaging in trauma informed care. Given how few individuals report sexual violations, it’s hard to have much faith in this approach. This depends on the victim declaring herself vulnerable in order to modify the behaviour of the staff. Is the client who does not expose her previous violations not afforded the same concessions of dignity, consent and trauma informed care?
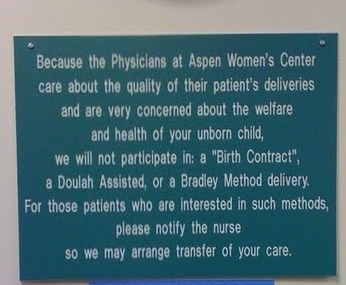
And it’s not just hospitals where survivors are fighting to have their dignity and their rights respected. Home birth clients who have engaged a midwife can also experience the same difficulties in ensuring an appropriate trauma informed approach. A pregnant mother planning a home birth contacted Birth Trauma Ontario with this message: "I'm 37+3 and I met with my midwives this morning and they would like to terminate our relationship because they are concerned about the tone of my birth plan and feel that I am placing my baby in danger by declining routine pelvic exams during labour. What the f*ck do I do?" The mother was open to checks if there is a reason but didn't want regular exams every few hours. The midwife terminated their relationship shortly after her client sent this message.
When birthing clients register complaints about procedures done unnecessarily or without consent or after consent was removed, the typical response from the hospital or the regulatory body is that she didn’t understand what happened to her. She's told her provider was saving hers and her baby’s life. And she ought to be grateful. It’s one of the supremest forms of gaslighting and birthing women experience it all the time. Even in general society, when a mother talks about how difficult or traumatic her birth was or that her wishes were disregarded, the usual response is that she should be grateful, as the baby is all that matters. Somehow, we think babies can thrive with broken mothers if they just ignore their own needs enough.
Giving birth is pretty much the same, physiologically speaking, across most mammals, including humans. However, how we do birth is wholly cultural. In this culture of #metoo, women are expected to submit to routines and procedures that expose them, frighten them, penetrate them, and rob them of their dignity because it’s what women do to have a baby. Asking for a better experience is called selfish.
Rape culture affects all of us and it’s pervaded the delivery room where men sometimes still “joke” about a “husband stitch” to make her perineum nice and tight for the pleasure of the penis that will penetrate her after her recovery. Where women are still forced to birth on their backs in order to accommodate the skills limitations of the paid provider. Where strangers come and go. Where she receives routine cervical checks that are primarily for the benefit of the institution’s time and resource management. Where she is given no choice regarding the birth of her breech baby. Where she still hears providers pull the dead baby card in order to gain her compliance.
When Tarana Burke talks about how #metoo has gone viral, she is concerned whether those who helped to inspire women to disclose their stories of survival are prepared for what comes next.
There are many of us who are prepared. We understand that sexual violation writes on the fabric of who you are. We know that you sometimes want more time to choose your path – for birth and beyond without arbitrary time limits. We know that you don’t trust everyone, including yourself at times. We know that you have been manipulated and need to know that no one will use manipulation or coercion to gain your compliance. We know that you don’t want to be insulted by being told to stay off the internet. We understand that safety is more than a baby who is alive at the end of the process. It’s also about whether your spirit and your soul are alive as well. We know that you have requirements for your dignity and they may not be the same as your neighbour’s. We know that you don’t respect threats, lies or coercion. We know that if there’s going to be a power imbalance in the relationship, then you are the one with the power. We ask you for your truth as that’s more relevant that a practice guideline or a study.
As individuals are still reeling from the massive participation and revelation in the #metoo campaign, this is a good time to consider how we treat each other when it comes to personal boundaries and intimacy. Pregnancy, birth, and breastfeeding are deeply personal and intimate experiences. It’s time to take a good look at our rape culture for what it is and to begin to connect with birthing clients in a way that honours each one’s dignity, experiences and boundaries. We need to work together to ensure birthing families have real choices that respect their history, their values, their future, their hopes and their identity.
And for every person who said #metoo, there are hundreds and thousands more who didn’t say it but have experienced it nonetheless. Let’s be kind together and help each other heal. And let’s help each other to experience birth in a new culture of love and respect. Let’s learn the art of trauma informed care and learn to ask better questions and to offer options that really support each other. Together we are stronger.
Much love,
Mother Billie
References
Bates, C. K., Carroll, N., & Potter, J. (2011). The challenging pelvic examination. Journal of general internal medicine, 26(6), 651-657.
Bowser, D., & Hill, K. (2010). Exploring evidence for disrespect and abuse in facility-based childbirth. Boston: USAID-TRAction Project, Harvard School of Public Health
Clarke, E. (2015). Law and Ethics for Midwifery. Routledge.
Faravelli, C., Giugni, A., Salvatori, S., & Ricca, V. (2004). Psychopathology after rape. American Journal of Psychiatry, 161(8), 1483-1485.
Perkins, B. B. (2004). The medical delivery business: Health reform, childbirth, and the economic order. Rutgers University Press.
Halvorsen, L., Nerum, H., Øian, P., & Sørlie, T. (2013). Giving birth with rape in one's past: a qualitative study. Birth, 40(3), 182-191.
Reed, R., Sharman, R., & Inglis, C. (2017). Women’s descriptions of childbirth trauma relating to care provider actions and interactions. BMC pregnancy and childbirth, 17(1), 21.
Robohm, J. S., & Buttenheim, M. (1997). The gynecological care experience of adult survivors of childhood sexual abuse: a preliminary investigation. Women & health, 24(3), 59-75.
Roth LM, Heidbreder N, Henley MM, Marek M, Naiman-Sessions M, Torres J and Morton CH. (2014). Maternity Support Survey: A Report on the Cross-National Survey of Doulas, Childbirth Educators and Labor and Delivery Nurses in the United States and Canada.
The epic failure of the evidence-based movement
“All procedures offered to a mother should be researched by herself so she can make an informed decision.”
(posted on Facebook on a thread about routine interventions)“Make sure you hire a doula.”
(said by everyone)
Why are mothers being told to do their own research, find out more about their provider and their hospital, check out the alternatives, and make sure they can make an informed decision?
The pipe on my hot water tank sprung a leak and I called a plumber. Not once was I admonished to check into the possible things he might do to fix it and to decide if it was evidence based or if I should switch plumbers. He did a good job because if he didn’t, it would get around, and no one would hire him again.
And yet, mothers are urged to make sure they find out for themselves the risks of ultrasounds, what the science says about postdates, the risks of synthetic oxytocin (Pitocin/syntocinon), whether an epidural can cause problems, whether Friedman’s curve is actually useful for deciding on a “failure to progress” or if it’s a tool for the hospital to manage their time and resources, whether an induction for a big baby is evidence based, or if their provider supports a VBAC and what the risks are between VBAC and a repeat c-section. And if nothing else, hire a doula. And on it goes.
What’s behind this push for families to do their own research into the routines and interventions of birth? I think it’s been the epic failure of the evidence-based movement.
“All procedures offered to a mother should be researched by herself so she can make an informed decision.”
(posted on Facebook on a thread about routine interventions)
“Make sure you hire a doula.”
(said by everyone)
Why are mothers being told to do their own research, find out more about their provider and their hospital, check out the alternatives, and make sure they can make an informed decision?
The pipe on my hot water tank sprung a leak and I called a plumber. Not once was I admonished to check into the possible things he might do to fix it and to decide if it was evidence based or if I should switch plumbers. He did a good job because if he didn’t, it would get around, and no one would hire him again.
And yet, mothers are urged to make sure they find out for themselves the risks of ultrasounds, what the science says about postdates, the risks of synthetic oxytocin (Pitocin/syntocinon), whether an epidural can cause problems, whether Friedman’s curve is actually useful for deciding on a “failure to progress” or if it’s a tool for the hospital to manage their time and resources, whether an induction for a big baby is evidence based, or if their provider supports a VBAC and what the risks are between VBAC and a repeat c-section. And if nothing else, hire a doula. And on it goes.
What’s behind this push for families to do their own research into the routines and interventions of birth? I think it’s been the epic failure of the evidence-based movement.
Evidence-based medicine
The expression “evidence-based medicine” was introduced in 1991 in an ACP (American College of Physicians) Journal Club editorial and was quickly embraced. Medical clinical practice has been historically referred to as the “art of medicine” where expert opinion, experience and authoritarian judgement were the foundation for decision-making. Medicine held a strong distrust of biomedical research, scientific methodology and statistical analysis (Sur & Dahm, 2011). The problem was that medicine was lagging in accuracy and safety as other disciplines embraced these scientific tools. Obstetrics, in particular, was the medical discipline with the least sound practices, so much so, that Archie Cochrane awarded the discipline of obstetrics with the humiliating “wooden spoon” award in 1979. A decade later, A Guide to Effective Care in Pregnancy and Childbirth was published which seemed to usher in a new approach in obstetrics, and he agreed that it was time to withdraw his insult.
The most widely-accepted definition of evidence-based medicine is as follows:
“Evidence-based medicine [or care] is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research” (Sackett, 1996).
This sounds like the ideal where clients are both treated as individuals and are informed by the most current scientific information. However, this is not the experience of birthing mothers. Instead, mothers throughout the world, where obstetricians are the primary providers and hospitals are the primary birth location, are treated to what is largely a one-size-fits-all approach that resembles Henry Ford’s invention of the assembly line manufacturing plant (Perkins, 2004).
Policies that benefit the institution and the provider have replaced both common sense and holistic care. The widespread ban on VBACs (vaginal births after caesareans) in the US and the near universal unwillingness to support a vaginal breech birth speaks to the profit-before-sense kind of treatment that force women into increasingly unnecessary and risky surgeries without choice or individual care.
It’s also important to consider the limitations of “evidence-based” research. The randomised controlled trial (RCT) has been decided by committee to be the gold standard in research methodology. What this fails to recognise is that a birthing mother is an autonomous human who needs to be given a right to say what happens to her in birth. It’s unethical to randomly assign her to one arm of a research study without her ability to know what her choices are and to make an informed decision. Further, funding drives research. Only certain studies receive funding, which seldom extends beyond a brief time period. When interpreting research, one must consider the question being asked, the conditions under which it was asked, the parameters of the study, potential biases, limitations, and often, false conclusions (Ioannidis, 2005).
Increasing interventions
In the last several years, the rate of obstetrical interventions has increased dramatically without corresponding benefit. Increased interventions in low-risk mothers show an increase in neonatal morbidity (Dahlen et al., 2014). One would think that the evidence-based approach to maternity care would mean a reduced incidence of sick or hurt babies. Instead, money and profit has been a powerful motivator for increased use of interventions. It’s a well-documented fact that a mother in a private facility is more likely to have increased interventions and caesarean surgery than in a public facility. In other words, she’s more likely to have expensive services, like surgery, when she (or her insurance) has more money to offer (Dahlen et al., 2012).
Medical malpractice liability is another factor that influences the high rates of interventions and lessens the choices and autonomy provided to mothers. When the clinician or the facility is worried about being sued, they are more likely to use interventions and perform surgery (Morris, 2015).
Further, there is a direct relationship between a surgeon’s malpractice premiums and the rate of caesarean surgeries. In other words, the more that the provider pays for insurance, the more that caesarean surgeries are performed and the fewer VBACs that are supported (Yang, Mello, Subramanian, & Studdert, 2009).
The rates of interventions vary widely across countries, regions and even hospitals, including caesareans (Kozhimannil, Law, & Virnig, 2013), episiotomies (Graham, Carroli, Davies, & Medves, 2005), inductions (Tenore, 2003), and most every obstetric intervention. Certainly, differences in clientele would influence the rates of interventions in that a mother who is not well would have complications that require medical support. However, even that cannot explain the wide variation in obstetric interventions. The primary predictor of whether a low risk mother will receive a routine intervention is the kind of provider she has (Robinson, Norwitz, Cohen, & Lieberman, 2000).
Outdated practices
ACOG (American Congress of Obstetricians and Gynecologists) themselves admit that only about 25% of their obstetrical practice guidelines are based in good quality research. The rest is based in poor quality studies, opinion, and habit (Wright et al., 2011). The SOGC’s (Society of Obstetricians and Gynaecologists of Canada) practice guidelines are not much different in content. And frankly, no matter what the evidence says, most mothers get what’s offered and that’s often outdated protocols based on poor quality information, or habit.
We’ve known for 30 years that routine episiotomy, cutting the perineum to make a larger passage for the baby at birth, causes increased 3rd and 4th degree lacerations, increased fecal incontinence, and increased pain that can last years (Thorpe, Bowes Jr, Brame, & Cefalo, 1987; Borgatta, Piening, & Cohen, 1989; Klein et al., 1992; Signorello, Harlow, Chekos, & Repke, 2000; Hartmann et al., 2005). While the rate of episiotomies has been falling in most locations, according to the Listening to Mothers III Survey (US), 17% of women still had this procedure (Declercq, Sakala, Corry, Applebaum, & Herrlich, 2013).
“During the 40 minutes of pushing, the doctor turned to my mother and said, “I’m cutting her” and I yelled and begged for her NOT to cut me. But she ignored me and did it anyways. When she started to stitch me up, once again, I was screaming and begging for her to stop because it was extremely painful. I didn’t even know they were supposed to numb you first until recently.” (Carol, personal communication, 2016)
Back in the 1940’s it became routine to deny a mother any food in labor since she was going to be put under general anesthesia for her birth. The concern was that she would vomit under anesthesia and then aspirate (breathe) in the vomit and possibly die from the complications. Interestingly, it’s also been know for almost 30 years that fasting during labour doesn’t ensure gastric emptying (an empty stomach) and instead increases the acidity in her stomach, which is more problematic. And in fact, the likelihood of a mother dying from aspirating vomit during an emergency caesarean under general anesthesia is about 7 in 10,000,000 births (Sleutel & Golden, 1999). Further, forced fasting leads to a longer pushing stage (Rehamani, Khakbazan, Yavari, Granmayeh, & Yavari, 2012). No doubt that’s because labour burns up to 1000 calories per hour and the mother just gets tired from lack of nourishment.
The original recommendation in the 1940’s was based on worry and an attempt to exercise caution. There has been no corroborating evidence since then and any research has shown that eating and drinking brings comfort to mothers and reduces both pain and length of labour, so there is no reason to restrict the food they want (Singata, Tranmer, & Gyte, 2010). And yet, most mothers are not “allowed” to eat during labour when they birth in a hospital due to outdated and inflexible policies. Adding in a routine IV with glucose to replace real food just increases problems, as those newborns are more likely to have serious low blood sugar (Grylack, Chu, & Scanlon, 1984). So why aren’t most mothers eating in labour? Because hospitals don’t change outdated practices when it’s still working for them. Not providing food for labouring mothers saves money.
There are so many non-evidence based routines happening every day including:
Caesareans for failure to progress based on outdated time limits (Laughon, Branch, Beaver, & Zhang, 2012)
Routine induction at early term with a membrane stripping (Hill et al., 2008)
Routine induction for suspected fetal macrosomia (big baby) (Boulvain, Irion, Dowswell, & Thornton, 2016)
Induction for isolated (no other medical complications) oligohydramnios (low amniotic fluid) at term (close to your due date) (Manzanares et al., 2007)
Induction for isolated (no other complications) hypertension (high blood pressure) near term (Broekhuijsen et al., 2015)
Birthing on your back with your feet in the air or in stirrups, called a supine delivery (Terry, Westcott, O'Shea, & Kelly, 2006)
Staying in bed for labour (Bloom et al., 2008)
Continuous electronic fetal monitoring (Alfirevic, Devane, & Gyte, 2013)
Mandatory surgery for a breech presentation (Louwen, Daviss, Johnson, & Reitter, 2016)
Immediate cord clamping (Hutton, Reitsma, & Kaufman, 2007)
And on it goes.
“I remember telling my first doctor that I didn’t want or need rhogam at 27 weeks. I had researched it and because both my husband and I were negative blood type, it was impossible to have a positive baby. She told me I had no choice. It was mandatory.” (Joanne, personal communication, 2016)
How bad is it?
Consider that in the survey, Listening to Mothers III (US) (Declercq et al., 2013)
80% did not eat during labour
68% of mothers birthed on their backs
55% did not walk or move around during active labour
44% were induced for the reason that they were merely at term
16% were induced because the doctor was worried about a large baby
11% were induced because the doctor was worried about low fluid at term
10% had their public hair shaved for a vaginal birth
and when making a decision to have a repeat c-section rather than attempt a VBAC 63% said it was the doctor who made the decision
According to BORN Ontario (Niday Perinatal Database) 2005-2006 to 2009-2010 (BORN, 2011)
Inductions have risen from 21.8% in 2005-6 to 25.2% in 2009-10. A 15.6% increase in just 4 years cannot be explained by a massive shift in maternal-fetal wellbeing, but rather speaks to how quickly practitioners choose an intervention on a broad scale.
The rate of repeat c-sections increased 28.6% over that same time period
57.6% of elective repeat caesareans were performed before 39 weeks
18.3% of mothers had an episiotomy.
The caesarean section rate has increased every year across Canada from 18.7% in 1997 to 27.5% in 2014 where repeat surgery makes up more than half of this rise (CIHI, 2016). It seems that scheduled, profitable, daylight obstetrics is the driver behind this as there has been no new evidence of increased risk or harm to mothers or babies from VBAC births in the last several years.
What is stunning is that in spite of the evidence based movement, maternal mortality has risen in the US between 1990 and 2013 from 12 deaths per 100,000 to 28 per 100,000. Lack of consistent obstetrical practices has been identified as a major concern in this rising rate (Agrawal, 2015). And given the high rates of caesarean surgery, often due to policy or insurance premiums, it’s necessary to count the cost in lives lost due to excessive rates of surgery. Postpartum death is 3.6 times higher after a surgical birth than a vaginal birth (Deneux-Tharaux, Carmona, Bouvier-Colle, & Bréart, 2006).
In Canada, maternal mortality increased from 6 per 100,000 in 1990 to 11 per 100,000 in 2013. The question that begs to be answered is, where does the shocking increase in surgical birth fit into this decline in maternal safety?
Obstetric violence
In 2007, Venezuela became the first country to define obstetric violence through the Organic Law on the Right of Women to a Life Free of Violence.
In this law, obstetric violence is defined as:
“The appropriation of the body and reproductive processes of women by health personnel, which is expressed as dehumanized treatment, an abuse of medication, and to convert the natural processes into pathological ones, bringing with it loss of autonomy and the ability to decide freely about their bodies and sexuality, negatively impacting the quality of life of women.”
The following acts, executed by care providers, are considered obstetric violence:
1. Untimely and ineffective attention of obstetric emergencies;
2. Forcing the woman to give birth in a supine position, with legs raised, when the necessary means to perform a vertical delivery are available;
3. Impeding the early attachment of the child with his/her mother without a medical cause thus preventing the early attachment and blocking the possibility of holding, nursing or breast-feeding immediately after birth;
4. Altering the natural process of low-risk delivery by using acceleration techniques, without obtaining voluntary, expressed and informed consent of the woman;
5. Performing delivery via cesarean section, when natural childbirth is possible, without obtaining voluntary, expressed, and informed consent from the woman.
Obstetric violence is global and systemic (WHO, 2014). Having procedures performed that introduce risk without their knowledge or consent routinely violates mothers. Having her membranes broken in a healthy labour without indication, or having synthetic oxytocin unknowingly introduced into their IV, being forced onto her back for delivery, or having her genitals cut against her wishes are just the tip of the iceberg.
And yet, no one is holding the industry accountable. Obstetrical societies (ACOG, SOGC, et. al.) maintain a powerful lobbying presence with government to ensure that public policies and government spending are favourable to their industry. An absence of adequate oversight has allowed this industry to escalate their intrusion into healthy pregnancies to the point where 1 in 3 mothers say their births were traumatic and up to 1 in 10 mothers are grappling with postpartum PTSD as a result of their birthing experience (Beck, Gable, Sakala, & Declercq, 2011).
“I had a successful VBAC in a hospital. The next thing I know, an entire arm, up to her elbow, shoots into my vagina and uterus without any warning. I felt every inch of my placenta being ripped out of my uterus. I screamed at her to stop. Instead, the nurse pinned me down. PTSD robbed me of the next year of my life.” (Marie, personal communication, 2016)
The fact that the industry will not hold those providers and those institutions accountable for dangerous, outdated, and at times, abusive practices is simply stunning. Lateral violence (bullying, insults, coercion, sabotage, and even physical assault) within the industry keeps whistle blowers from speaking up, in particular nurses (Jackson et al., 2010). Nurses are especially vulnerable to lateral violence as the vast majority of nurses have been victims, most often from senior nurses (Christie, Jones, & PMHNPBC, 2014). This impacts their delivery of care to their patients and patient safety. In hospitals, nurses are the primary contact with the birthing family and the one in the best position to advocate for her patient and to report abusive or outdated care. Abusive behaviour within the nursing profession has contributed to preventing them from appropriately dealing with this failure on the part of the industry to give mothers the care they need and deserve.
The birth monopoly
Through clever marketing and expensive lobbying, obstetrics has gained a monopoly on birth. In most developed nations, hospitals have cornered the market on birth services and obstetricians, although more expensive and associated with more adverse outcomes in low risk populations, are the primary provider for most women. In places where midwifery is integrated into the health system, meaning they can facilitate a transfer to a hospital where her client will be accepted and the transfer is respectful and seamless, mothers have better outcomes at home with a midwife (Hutton, Reitsma, & Kaufman, 2009).
Physicians themselves are punished for providing true family centred care and risk losing hospital privileges for supporting a homebirth where the money doesn’t reach the institution. Like a dangerous cult, adherents (obstetricians) have even pursued a court order to force a mother to undergo mandatory caesarean surgery or called in child protective services to apprehend the children of mothers who disobeyed their dictates (Diaz-Tello, 2016).
“After 2 attempted homebirths that ended in caesareans, I was told that no midwife or doctor would support plans to have a homebirth VBAC. I could attempt a hospital VBAC but I would have to “fight” for it. To plan to attempt a vaginal birth at the same hospital, knowing that I would have to resist the system and medical staff every step of the way, was a recipe for failure and emotional distress.” (Lainie, personal communication 2016)
A few good folks
This is an industry-wide problem. However, there are truly wonderful individual providers who are doing their best to provide sensitive and individualised care with the best information they have. And they deserve credit, respect and thanks. Both doctors and midwives are routinely refused the opportunity to serve their clients in the manner they wish, perhaps through offering vaginal breech support, or not inducing according to policy when there is no medical indication. Yet these brave providers offer this care in the face of potentially sabotaging their opportunities for career advancement.
These providers are in high demand and are sometimes vilified by their colleagues whose excessive interventions bring more money into the industry coffers. They are shining diamonds in a deep mine and they make a difference in the lives of those fortunate enough to find them.
Individual nurses have taken the brunt of institutional hostility for advocating for their clients, for reporting unsafe practices, and for holding their colleagues to a higher standard. These are the professionals who deserve support and accolades.
Indeed, the evidence-based movement has been an epic failure that has left families reeling from their inability to influence their providers or the system that has set itself up to “save” her and her baby.
Families are paying the price
The true failure of the evidence-based movement has been the toll exacted on birthing families through lack of autonomy, lack of choice, excessive interventions, excessive surgery, birth trauma, and lives lost.
Due to the failure of the industry to deliver on their promise, we’ve entered the age where evidence based-medicine has become the responsibility of the consumer. Birthing families are urged to learn what their provider won’t learn or won’t practice.
When they are caught in a system run by dinosaurs, they are told that they didn’t do their research, they didn’t hire a doula, or they didn’t advocate for themselves. And the industry eats this up. They tell mothers to come in with a birth plan, all the while knowing that they see a birth plan as a direct route to more interventions (Grant, Sueda, & Kaneshiro, 2009).
A switch to a midwifery model of care with midwives providing the bulk of maternity services would mitigate some of these issues, as they’re more likely to use evidence-based care and to engage in informed consent and mother-centred care (Sandall, Soltani, Gates, Shennan, & Devane, 2016). However, a profitable industry with well-paid lobbyists won’t give up power and control easily. Obstetrics is currently a one-stop shop that provides a drive-through experience where everyone gets what’s on the menu.
You’ll note that when drawing attention to the need for mothers to do their own research or cautioning them to learn more about their provider before they consent to a routine, we hear total nonsense from industry members about not scaring mothers, not spreading misinformation, going with the flow, staying off the internet, and trusting the professionals. What they should be doing is apologising for aiding and abetting outdated protocols and industry-favourable policies that hurt mothers and babies and that it’s time to hold themselves accountable and rise to a higher standard.
Indeed, the evidence-based movement has been an epic failure that has left families reeling from their inability to influence their providers or the system that has set itself up to “save” her and her baby.
"I left the care of midwives when I caught them in lies and practices that went against informed choice. Despite what the medical system would have you believe, I had a wonderful and safe VBAC at home without a medical professional." (Chahna, personal communication, 2016)
The grassroots move to a new paradigm
Humans are resilient and they’ve always found a way to step away from systems that feel oppressive and to form communities that chart a path that honours their values, despite the risk of persecution. The rise of the DIY (do it yourself) birth movement, also called freebirth, unassisted, or family birth is a grassroots response that sees families taking care of each other outside of the obstetrical industry. There’s been a rise in unassisted homebirths in Sweden, Australia, Canada, the US, and Finland in response to the biomedical approach to birth and lack of autonomy for birthing mothers (Holten & de Miranda, 2016).
Of course, the obstetrical industry sees this as an exceptionally dangerous movement. Yet, their warnings may not match up with the experiences of the families themselves and may be more related to their position as a monopoly than the evidence of the safety of birth outside of their oversight.
In an anonymous online survey from December 2014 until September 2015, mothers who planned an unassisted birth responded (O’Day, 2016).
857 respondents from around the world
1449 babies born
1444 births (5 sets of twins)
1339 babies were born “unassisted”, meaning that there was no licensed attendant present although there might have been family, friends, doulas, or unregistered midwives.
The primary reason for choosing an unassisted birth was that they were led by their intuition (80.24%). The next most common reason was their dislike of hospitals (77.32%). They were also concerned for their newborn’s safety within a hospital setting (72.2%) and did not want to repeat a prior bad hospital experience (51.83%).
The results were interesting in the extraordinarily positive outcomes.
There were no maternal deaths
The neonatal death rate was 2.2 per 1000, which is comparable to the US rate of 2.97 per 1000
The caesarean rate was 1.24%
Of those who attempted a VBAC, 100% achieved it
Of those who had a VBAC, just over one quarter had had more than one previous caesarean
One third of the mothers had no prenatal services with a licensed provider, also called ‘prenatal care’ (this doesn’t account for community care and wellness measures)
Over 70% had no monitoring throughout labour and birth, i.e. no one listening to the baby’s heartbeat or routine vaginal exams
Just over 2% transported the newborn to a medical facility within the first week, mostly for breathing concerns
3.52% of the mothers transported for medical help after the baby was born primarily for postpartum haemorrhage
Certainly, this is a self-selecting group who responded to this survey. However, given that some of them were “high risk” in that they had had previous caesareans, had no prenatal care, and 5 were expecting twins, these results are seldom found within the medical obstetrical industry.
Once I decided not to continue prenatal care with the registered midwives, I was easily able to avoid trauma triggers and enjoy my pregnancy a lot more. The birth of my third baby was awesome! I was free to move around the whole house, I could eat or drink when I felt like it, I didn't have a single exam and I slept when I felt tired. I wasn't alone, but the people who were there didn't disturb me in any way. I never once wanted drugs for pain or to go to the hospital, it wasn't an option for me. My daughter had the best birth. No trauma, drama, drugs, strangers or tearing. Just a simple, healthy, happy family birth. (Samantha, personal communication, 2016)
© Billie Harrigan Consulting
As consumers have come to understand that the onus for evidence-based medicine has fallen on their shoulders, they’ve responded with outreach and connection. Online groups connect families to each other where they share research, studies, tips and encouragement. They share their medical history with one another and offer suggestions for self-care as well as recommendations for those providers and traditional birth attendants who support clients with holistic and scientifically sound care.
In-person groups are gathering to teach one another the physiology of birth, the mechanics of a vaginal breech birth, how to resolve a shoulder dystocia or a head entrapment, and to practice neonatal resuscitation skills.
Doulas are investing in advanced education and research skills to support their clients’ wishes for the evidence, access to their provider’s practice guidelines, and community connections and alternative care. Doulas are becoming specialists in supporting self-advocacy, research-based information, and helping clients connect to the services they need and want.
And as we learn more, we’re also discovering the importance of our microbiome and the epigenetic expression of our DNA where today’s one-size-fits-all comes across as pure buffoonery.
Taking back birth
We are at a crossroads in human history that will unfold over time. The “take back birth” movement is gaining momentum and this is being met with religious like zeal from the industry and its adherents in its opposition. They preach a different gospel where the modern medicalisation of birth and wholesale institutionalisation of birthing women has “saved” them. It’s a gospel that doesn’t hold up to scrutiny but nonetheless forms the lexicon of our culture (Tew, 2013).
So what can families do in light of the epic failure of evidence-based medicine?
Perhaps the answer lays in common sense.
Common sense dictates that if frequent prenatal visits and testing is upsetting, that the individual could just choose to bypass many of them. Science affirms that prenatal testing, no matter the results, increases maternal anxiety (Allison, Stafford, & Anumba, 2011). Prenatal anxiety is a risk factor for postpartum PTSD after a traumatic birth (Söderquist, Wijma, Thorbert, & Wijma, 2009). Maternal anxiety is also associated with poorer birth outcomes (Kumari & Joshi, 2014). And skipping those visits actually has no adverse outcome on the mum and baby and only affects the provider’s pocketbook (Walker, McCully, & Vest, 2001).
Common sense tells us that if a technology is useful for breaking up tissues such as cysts, scar tissue or kidney stones because it moves cells, then it might not be entirely safe for developing fetuses. Many parents are wary of ultrasound and their instincts tell them to bypass this routine. In fact, routine and frequent ultrasounds can contribute many problematic issues and has still not shown any benefit to mothers and babies, however it does increase inductions and caesareans (Cohain, 2011).
Common sense tells us that if we don’t want the gloved hand of someone we’re not in an intimate relationship with in our vaginas, we might want to decline as it may be more problematic than helpful (Lenihan, 1984).
Common sense suggests that if a hospital isn’t your cup of tea then birthing at home is a reasonable option (NICE, 2014).
Common sense and science are often aligned beautifully and generally support an individualistic approach to wellness, including birth, which takes into account a birthing mother’s physical, social, spiritual, and relational complexities. And as we learn more, we’re also discovering the importance of our microbiome and the epigenetic expression of our DNA where today’s one-size-fits-all comes across as pure buffoonery.
It’s going to be interesting to see how the medical industry responds to this growing grassroots movement. No doubt, lobbyists will pursue legislation to force mothers into the system for profit under the guise of “safety” which will drive families deeper underground. And should the numbers of families who choose to give birth outside the system actually have an impact on the profit margin of hospitals and obstetrical practices, then we’ll see a swift shift to “evidence-based” and “family-centred” care.
Until then, those good providers will do the best they can. Doulas will equip their clients with science and resources. And families will connect to support one another on this journey.
Evidence-based care has been an epic failure for parents but a mighty gold strike for the industry as they’ve cashed in on an illusion.
“I wish I knew then that I had the power to say NO. This is my body and we’re going to do this my way.” (Janice, personal communication, 2016)
References
Agrawal, P. (2015). Maternal mortality and morbidity in the United States of America. Bulletin of the World Health Organization, 93(3), 135-135.
Alfirevic, Z., Devane, D., & Gyte, G. M. (2013). Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. The Cochrane Library.
Allison, S. J., Stafford, J., & Anumba, D. O. (2011). The effect of stress and anxiety associated with maternal prenatal diagnosis on feto-maternal attachment. BMC women's health, 11(1), 1.
Beck, C. T., Gable, R. K., Sakala, C., & Declercq, E. R. (2011). Posttraumatic stress disorder in new mothers: Results from a two‐stage US National Survey. Birth, 38(3), 216-227.
Better Outcomes Registry & Network (BORN) Ontario. (2011). Perinatal Health Report 2009-2010. Greater Toronto Area (GTA) - LIHNs 5 to 9. Ottawa ON.
Bloom, S. L., McIntire, D. D., Kelly, M. A., Beimer, H. L., Burpo, R. H., Garcia, M. A., & Leveno, K. J. (1998). Lack of effect of walking on labor and delivery. New England Journal of Medicine, 339(2), 76-79.
Borgatta, L., Piening, S. L., & Cohen, W. R. (1989). Association of episiotomy and delivery position with deepperineal laceration during spontaneous delivery in nulliparous women. American journal of obstetrics and gynecology, 160(2), 294-297.
Boulvain, M., Irion, O., Dowswell, T., & Thornton, J. G. (2016). Induction of labour at or near term for suspected fetal macrosomia. The Cochrane Library.
Broekhuijsen, K., van Baaren, G. J., van Pampus, M. G., Ganzevoort, W., Sikkema, J. M., Woiski, M. D., ... & Rijnders, R. J. (2015). Immediate delivery versus expectant monitoring for hypertensive disorders of pregnancy between 34 and 37 weeks of gestation (HYPITAT-II): an open-label, randomised controlled trial. The Lancet, 385(9986), 2492-2501.
Canadian Institute for Health Information, & Canadian Population Health Initiative. (2016). Improving the Health of Canadians. Summary Report [electronic Resource]. Canadian Institute for Health Information.
Christie, W., Jones, S., & PMHNPBC, R. (2014). Lateral violence in nursing and the theory of the nurse as wounded healer. OJIN: The Online Journal of Issues in Nursing, 19(1).
Cohain, J. S. (2011). Prenatal ultrasound does not improve perinatal outcomes. Midwifery today with international midwife, (102), 46-7.
Dahlen, H. G., Tracy, S., Tracy, M., Bisits, A., Brown, C., & Thornton, C. (2012). Rates of obstetric intervention among low-risk women giving birth in private and public hospitals in NSW: a population-based descriptive study. BMJ open, 2(5), e001723.
Dahlen, H. G., Tracy, S., Tracy, M., Bisits, A., Brown, C., & Thornton, C. (2014). Rates of obstetric intervention and associated perinatal mortality and morbidity among low-risk women giving birth in private and public hospitals in NSW (2000–2008): a linked data population-based cohort study. BMJ open, 4(5), e004551.
Declercq, E. R., Sakala, C., Corry, M. P., Applebaum, S., & Herrlich, A. (2013). Listening to MothersSM III.
Deneux-Tharaux, C., Carmona, E., Bouvier-Colle, M. H., & Bréart, G. (2006). Postpartum maternal mortality and caesarean delivery. Obstetrics & Gynecology, 108(3, Part 1), 541-548.
Diaz-Tello, F. (2016). Invisible wounds: obstetric violence in the United States. Reproductive Health Matters.
Graham, I. D., Carroli, G., Davies, C., & Medves, J. M. (2005). Episiotomy rates around the world: an update. Birth, 32(3), 219-223.
Grant, R., Sueda, A., & Kaneshiro, B. (2009). Expert opinion vs. patient perception of obstetrical outcomes in laboring women with birth plans. The Journal of reproductive medicine, 55(1-2), 31-35.
Grylack, L. J., Chu, S. S., & Scanlon, J. W. (1984). Use of intravenous fluids before caesarean section: effects on perinatal glucose, insulin, and sodium homeostasis. Obstetrics & Gynecology, 63(5), 654-658.
Hartmann, K., Viswanathan, M., Palmieri, R., Gartlehner, G., Thorp, J., & Lohr, K. N. (2005). Outcomes of routine episiotomy: a systematic review. Jama, 293(17), 2141-2148.
Hill, M. J., McWilliams, G. D., Garcia-Sur, D., Chen, B., Munroe, M., & Hoeldtke, N. J. (2008). The effect of membrane sweeping on prelabor rupture of membranes: a randomized controlled trial. Obstetrics & Gynecology, 111(6), 1313-1319.
Holten, L., & de Miranda, E. (2016). Women׳ s motivations for having unassisted childbirth or high-risk homebirth: An exploration of the literature on ‘birthing outside the system’. Midwifery.
Hutton, E. K., & Hassan, E. S. (2007). Late vs early clamping of the umbilical cord in full-term neonates: systematic review and meta-analysis of controlled trials. Jama, 297(11), 1241-1252.
Hutton, E. K., Reitsma, A. H., & Kaufman, K. (2009). Outcomes Associated with Planned Home and Planned Hospital Births in Low‐Risk Women Attended by Midwives in Ontario, Canada, 2003–2006: A Retrospective Cohort Study. Birth, 36(3), 180-189.
Ioannidis, J. P. (2005). Why most published research findings are false. PLoS Med, 2(8), e124.
Jackson, D., Peters, K., Andrew, S., Edenborough, M., Halcomb, E., Luck, L., ... & Wilkes, L. (2010). Trial and retribution: A qualitative study of whistleblowing and workplace relationships in nursing. Contemporary nurse, 36(1-2), 34-44.
Klein, M. C., Gauthier, R. J., Jorgensen, S. H., Robbins, J. M., Kaczorowski, J., Johnson, B., ... & Gelfand, M. M. (1992). Does episiotomy prevent perineal trauma and pelvic floor relaxation?. The Online journal of current clinical trials, 6019-words.
Kozhimannil, K. B., Law, M. R., & Virnig, B. A. (2013). Caesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Affairs, 32(3), 527-535.
Kumari, S., & Joshi, S. (2014). Birth outcomes following antenatal anxiety and depression.
Laughon, S. K., Branch, D. W., Beaver, J., & Zhang, J. (2012). Changes in labor patterns over 50 years. American journal of obstetrics and gynecology, 206(5), 419-e1.
Lenihan Jr, J. P. (1984). Relationship of antepartum pelvic examinations to premature rupture of the membranes. Obstetrics & Gynecology, 63(1), 33-37.
Lothian, J. (2006). Birth plans: the good, the bad, and the future. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 35(2), 295-303.
Louwen, F., Daviss, B. A., Johnson, K. C., & Reitter, A. (2016). Does breech delivery in an upright position instead of on the back improve outcomes and avoid caesareans?. International Journal of Gynecology & Obstetrics.
Manzanares, S., Carrillo, M. P., Gonzalez-Peran, E., Puertas, A., Montoya, F., Manzanares, S., ... & Montoya, F. (2007). Isolated oligohydramnios in term pregnancy as an indication for induction of labor. The Journal of Maternal-Fetal & Neonatal Medicine, 20(3), 221-224.
Morris, T. (2013). Cut it out: the C-section epidemic in America. NYU Press.
National Institute for Health and Care Excellence (NICE). (2014) Intrapartum care for healthy women and babies. Clinical guideline CG190.
O’Day, Katharine L. (2016). “Outside the System”: Motivations and Outcomes of Unassisted Childbirth. Published Online November 19, 2016, Sacred Transitions Midwifery Institute.
Perkins, B. B. (2004). The medical delivery business: Health reform, childbirth, and the economic order. Rutgers University Press.
Rahmani, R., Khakbazan, Z., Yavari, P., Granmayeh, M., & Yavari, L. (2012). Effect of oral carbohydrate intake on labor progress: randomized controlled trial. Iranian journal of public health, 41(11), 59.
Robinson, J. N., Norwitz, E. R., Cohen, A. P., & Lieberman, E. (2000). Predictors of episiotomy use at first spontaneous vaginal delivery. Obstetrics & gynecology, 96(2), 214-218.
Sackett, D. L. (1997, February). Evidence-based medicine. In Seminars in perinatology (Vol. 21, No. 1, pp. 3-5). WB Saunders.
Sandall, J., Soltani, H., Gates, S., Shennan, A., & Devane, D. (2016). Midwife‐led continuity models versus other models of care for childbearing women. Cochrane database of systematic reviews, (4).
Signorello, L. B., Harlow, B. L., Chekos, A. K., & Repke, J. T. (2000). Midline episiotomy and anal incontinence: retrospective cohort study. Bmj, 320(7227), 86-90.
Singata, M., Tranmer, J., & Gyte, G. M. (2010). Restricting oral fluid and food intake during labour. The Cochrane Library.
Sleutel, M., & Golden, S. S. (1999). Fasting in labor: relic or requirement. Journal of Obstetric, Gynecologic & Neonatal Nursing, 28(5), 507-512.
Söderquist, J., Wijma, B., Thorbert, G., & Wijma, K. (2009). Risk factors in pregnancy for post‐traumatic stress and depression after childbirth. BJOG: An International Journal of Obstetrics & Gynaecology, 116(5), 672-680.
Sur, R. L., & Dahm, P. (2011). History of evidence-based medicine. Indian Journal of Urology, 27(4), 487.
Tenore, J. L. (2003). Methods for cervical ripening and induction of labor. American family physician, 67(10), 2123-2128.
Terry, R. R., Westcott, J., O'Shea, L., & Kelly, F. (2006). Postpartum outcomes in supine delivery by physicians vs nonsupine delivery by midwives. The Journal of the American Osteopathic Association, 106(4), 199-202.
Tew, M. (2013). Safer childbirth?: a critical history of maternity care. Springer.
Thorp Jr, J. M., Bowes Jr, W. A., Brame, R. G., & Cefalo, R. (1987). Selected use of midline episiotomy: effect on perineal trauma. Obstetrics & Gynecology, 70(2), 260-262.
Walker, D. S., McCully, L., & Vest, V. (2001). Evidence‐based prenatal care visits: When less is more. Journal of Midwifery & Women’s Health, 46(3), 146-151.
World Health Organisation. (2014). The prevention and elimination of disrespect and abuse during facility-based childbirth: WHO statement.
Wright, J. D., Pawar, N., Gonzalez, J. S., Lewin, S. N., Burke, W. M., Simpson, L. L., ... & Herzog, T. J. (2011). Scientific evidence underlying the American College of Obstetricians and Gynecologists' practice bulletins. Obstetrics & Gynecology, 118(3), 505-512.
Yang, Y. T., Mello, M. M., Subramanian, S. V., & Studdert, D. M. (2009). Relationship between malpractice litigation pressure and rates of caesarean section and vaginal birth after caesarean section. Medical care, 47(2), 234.
The Textbook is Wrong
We were sitting across her kitchen table. A tissue was being nervously mangled in her trembling hands.
“I just can’t do it again,” she said. “Can you tell me about your daughter’s birth,” I asked her?
She explained that everyone told her it was a good birth. Her doctor said it was textbook perfect. Her mother was there and repeated her version of her granddaughter’s birth to everyone who would listen. It was natural. It was quick. It was the best day ever.
And as the story unfolded, tears welled up in my eyes, finally spilling down my own cheeks. It was an awful experience. And my heart broke into pieces again.
She described a birth where she was tortured with screamingly painful vaginal exams, weeping for them to stop, thrashing to escape the confines of the hospital bed where she was tethered to the monitoring machine for policy’s sake, begging to stand up, move, sway, anything to cope with her rapidly advancing labour. Her voice buried under a gentle shush so as not to scare the other mothers.
We were sitting across her kitchen table. A tissue was being nervously mangled in her trembling hands.
“I just can’t do it again,” she said. “Can you tell me about your daughter’s birth,” I asked her?
She explained that everyone told her it was a good birth. Her doctor said it was textbook perfect. Her mother was there and repeated her version of her granddaughter’s birth to everyone who would listen. It was natural. It was quick. It was the best day ever.
And as the story unfolded, tears welled up in my eyes, finally spilling down my own cheeks. It was an awful experience. And my heart broke into pieces again.
She described a birth where she was tortured with screamingly painful vaginal exams, weeping for them to stop, thrashing to escape the confines of the hospital bed where she was tethered to the monitoring machine for policy’s sake, begging to stand up, move, sway, anything to cope with her rapidly advancing labour. Her voice buried under a gentle shush so as not to scare the other mothers.
When the baby emerged, she was placed on her mother as the room cheered. Only, she felt nothing. Grateful that those hands wouldn’t enter her again, except in her dreams. The symptoms of PTSD followed her for the first year of her child’s life as she struggled to connect the version of her birth she’d been told and her personal experience of it.
And she just couldn’t do it again.
This is the story I hear over and over by mothers in all parts of the world. She’s told to be grateful for her healthy baby, to be grateful for the care she received, that her expectations were too high, that having a baby is hard and she had a low pain threshold, or that she was foolish for not taking the drugs offered her. She’s told anything except, “I’m sorry. It wasn’t meant to be that way.”
Research tells us that trauma is not particularly related to any emergencies or complications, but is dependent on how the mother experiences her birth. What can seem like a “textbook” birth to the clinician can be a devastating experience for the mother.
Birth is a hormonal process driven by our para-sympathetic nervous system, our “calm and connected” system. The primary driver of birth is oxytocin, which is the hormone of love, trust and bonding. Endorphins and prolactin ensure the experience is filled with pain-relief and joy. In today’s culture of fear, mothers are increasingly experiencing their births as traumatic as hospital policies serve the business end of cost-control, expediency, and insurance regulations. Doctors, nurses and midwives are sometimes constrained by policy in spite of the best interests of their clients.
Where birth is biologically programmed to be joyous, active, patient and primed for love and bonding, how we do birth in this culture is at odds with this biological imperative. The problem comes from what we call “textbook perfect”. The textbook is written from a medicalised perspective that is brand new in the biology of humans. Humans haven’t yet adapted to forced fasting, routine IVs, ultrasounds, continuous monitoring, hospital acquired infections, vaginal penetrations, forced on-her-back pushing, an inability to move and strangers between her legs.
When one third of mothers say their births were traumatic and one in ten struggle with PTSD, we know that birth is in crisis. And the textbook is wrong.
Of course, some births require medical assistance. Yet the question becomes, how can we protect a mother from trauma? And what happens when a pregnant mother says she can’t do that again?
In spite of the law that says a medical procedure cannot be performed on a non-consenting patient and that consent may be withdrawn at any point for any reason, the truth is that many things happen to a mother in labour in which she has no choice. In order to gain compliance, she may be told the baby might die. We call this ‘playing the dead baby card’ and it’s so common it’s becoming a laughing point.
There have been many a new textbooks written – from the mother’s perspective, from the baby’s perspective, from the vantage of good science, and yet mothers are still struggling. When a mother says she can’t do it again, it means we have to take a long hard look at what is happening today.
Strong and courageous leadership from medical associations including obstetricians, family physicians, nurses and midwives could lead the way in changing non-evidence based policies that serve the institution and insurance regulations but harm mothers and babies.
Mothers are increasingly learning the science of safe birth for themselves and are changing the conditions under which they give birth. Perhaps the quickest route to change is to spend our birthing dollars in those places that support the biology of birth and the law of informed consent and refusal.
It’s not selfish to want a great experience – it’s biology.